Archive : Article / Volume 2, Issue 1
- Review Article | DOI:
- https://doi.org/10.58489/2836-5917/008
Molecular Approach of Vascular Functions to Integrated Approach of Yoga Therapy: A Report
1.A-112, Type-V (Old), Uttar Pradesh University of Medical Sciences, P.O. Saifai, Etawah District. Uttar Pradesh State. India Pincode: 206130
Snehasis Bhunia
Citation: Snehasis Bhunia, (2023). Molecular Approach of Vascular Functions to Integrated Approach of Yoga Therapy: A Report. Clinical Cardiovascular Research. 2(1). DOI: 10.58489/2836-5917/008
© 2023 Snehasis Bhunia, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 30-12-2022
- Accepted Date: 12-01-2023
- Published Date: 01-03-2023
Physical Exercise; Yoga; Yoga Therapy; Vascular Physiology; cardiovascular diseases
Abstract
Integrated approach of yoga therapy (IAYT) is defined as the use of yoga practices for the prevention and treatment of medical conditions. Beyond the physical elements of yoga, this incorporates appropriate breathing techniques, mindfulness, and meditation in order to achieve the maximum benefits. The practice of yoga (IAYT) is not easy or as quick as taking medication, but mounting evidence suggest it is worth the effort and investment. This is based on Pancha kosha concept, helps one to reconnect with oneself. This can ultimately help to relieve one from the pressures and stressors which we receive almost daily. Neuroendocrine involvement is brought here and interactions between regulatory bodies and vascular functions have been elaborated. Only physical exercise or yoga did not show much beneficial. It is also should be noted that the field of yoga research encompasses the inherent dilemma of the wide variety of yogic practices used as interventional therapies. It has also been shown to have psychological benefits, as the practice can help to increase mental energy, positive feeling and decrease negative feeling of aggressiveness, depression and anxiety. Keeping these in minds it is very much essential to understand the regulatory involvement and their basic interactions with vascular physiology in IAYT.
Graphical Abstract
Introduction
It’s time to roll out your yoga mat and discover the combination of physical and mental exercises that for thousands of years have hooked yoga practitioners around the globe. The beauty of yoga is that you don’t have to be a yogi or yogini to reap the benefits. Whether you are young or old, overweight or fit, yoga therapy (IAYT) has the power to calm the mind and strengthen the body [1-2]. Yoga is for everyone.
Human body is made up by many organs. Organ is made up by many systems and again system is made up by tissues and again tissues are made up by cells. The human body has more than 30 trillion cells. A cell is surrounded by a membrane, which has receptors on the surface. A cell has several small structures inside it, including the nucleus, mitochondria, endoplasmic reticulum, and Golgi complex. These all have specific functions in the cell. This article is to bring out the mechanism involved in a cell while following a person yoga therapy (IAYT). This article is brought with basic information /link between Pancha kosha, regulatory systems and vascular physiology together which would be understood easily [2-7].
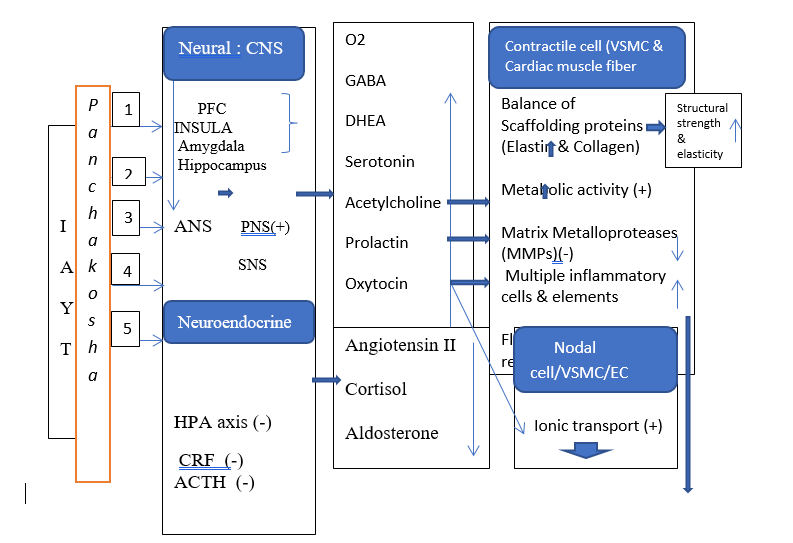
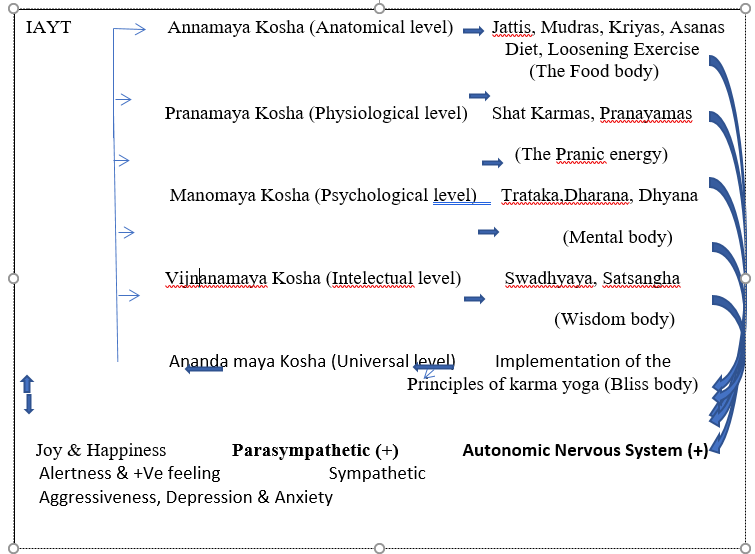
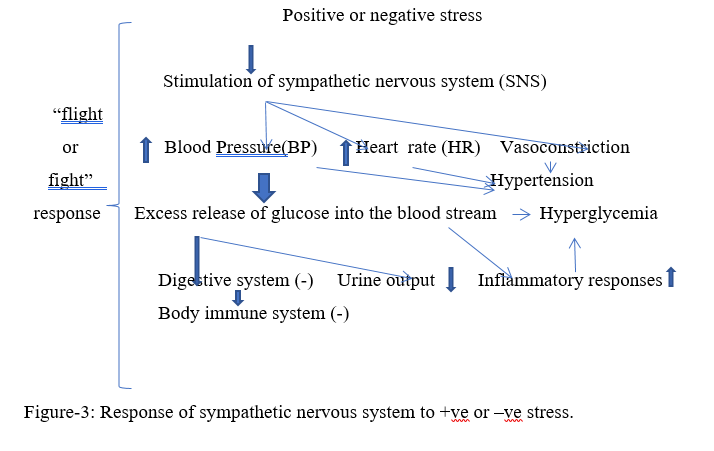
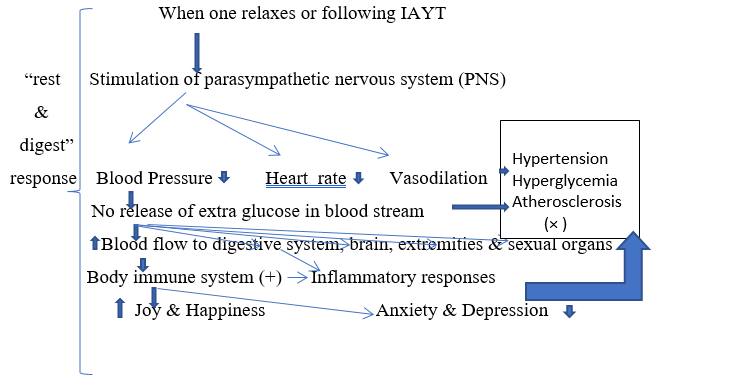
Integrated Approach of Yoga Therapy (IAYT) is an individualized, personalized and holistic approach that takes into account patient’s mind, body and spirit. This practice helps to diffuse anxiety and sadness, harmonizing system for the body, mind and spirit. Physical exercises, the physical components of yoga practices (only Asanas) and integrated approach to yoga therapy have several similarities, but also have important differences. Evidence suggests that IAYT appear to be superior to both physical exercise & yoga practices in most outcome measures. Emphasis on healthy life nourishing diet, a healthy and natural environment, a holistic lifestyle, adequate bodywork through Asanas, mudras and Kriyas, invigorating breath work through the use of pranayama and the production of a healthy thought process through the higher practices of Jnana and Raja yoga might be a more scientific and useful than only yoga (breath regulation, mindfulness during practice, and importance given to maintenance of postures) or physical exercise. The IAYT model is based on Pancha Kosa concept; various yogic practices are incorporated at each level to help subjects as therapeutic interventions with different disorders deal with their problems. IAYT bring the central nervous system (CNS), autonomic nervous system (ANS) into healthy balance by stimulating the parasympathetic nervous system (Figure-1). When our body & mind are threatened or perceives being stressed (+ve or –ve stress), sympathetic nervous system is stimulated (Figure-2), blood sugar level is gone up (Hyperglycemia). In contrast, opposite responses are observed when subject is at rest/relaxation or no stress (Figure-3).
To understand the mechanism, first, basic responsibility of sympathetic (Figure-3) and parasympathetic (Figure-4) is brought here and then, second, the route of therapy is highlighted one by one. In earlier reports, advantages of therapy or effect of therapy is discussed but underlying mechanism at molecular level has not been established [1-8]. We have reported some important findings related to IAYT [8-11].
Discussion
Basic regulatory pathways in IAYT: - Formal meditation practice can change both brain structure & function (7). Continuous practice can increase thickness of prefrontal cortex (PFC), amygdala, insular cortex (INSULA) & left hippocampus which have an active role in long term memory formation, emotional regulation & cognition [7]. This is done through stimulating autonomic nervous system (ANS). Regular surya namaskar yoga also can bring awareness &joy by stimulating parasympathetic nervous system (figure-2). ANS, both sympathetic (SNS) & parasympathetic (PNS) can act on endothelial cell (EC), vascular smooth muscle cell (VSMC), nodal & contractile cell in heart (Figure-2). Metabolic activity in these cells starts from binding with either adrenergic or cholinergic receptors. There may be a contraction & relaxation depends upon metabolic activity in the cells. Arterial compliance depends upon availability of gas transmitters (H2S, CO, & NO) which actually regulate the metabolic activities in these cells resulting vasoconstriction or vasodilation [9-10]. As a result, myocardial contractility, heart rate (HR), respiratory rate (RR) is altered and accordingly changes on blood pressure is also notified (Figure-2).
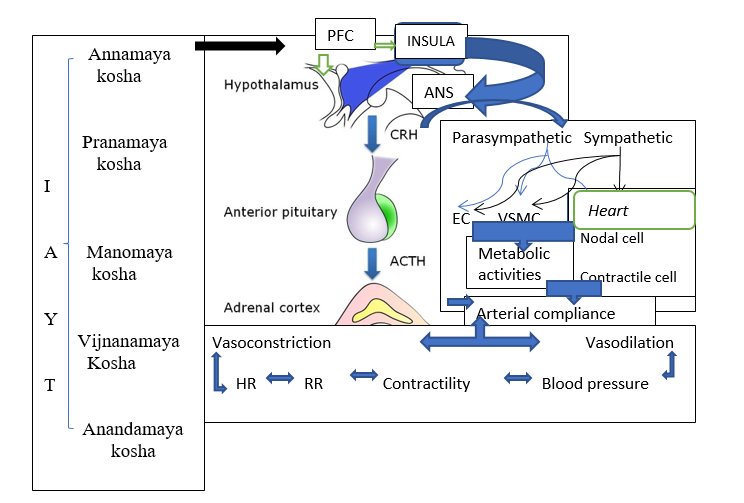
Several important alterations are noted while following ‘Pancha kosha’ (7). These are (1) Stimulation of muscle spindle & Golgi tendon organ (receptor for balance and tone), (2) Stimulation of vasomotor center, (3) Stimulation of central nervous system (CNS). All these together can involve autonomic nervous systems (PNS or SNS) (Figure-2). Endothelial cells (EC), Vascular smooth muscle cell (VSMC), nodal & contractile cell in heart are come into operation and the finale output depends upon either sympathetic (SNC) or parasympathetic (PNC) (Figure-2).
Hypothalamic-pituitary –adrenal (HPA) axis is also affected due to stimulation of limbic system (amygdala, hippocampus), Vascular responses depends on the secretion of corticotrophin- releasing factor (CRF), which act on pituitary for adrenocorticotropic hormone (ACTH) which subsequently stimulates the adrenal cortex for cortisol [7]. Effect of cortisol includes 1) increase blood sugar level leading to deterioration of balance between collagen and elastin- a main and important component for arterial compliance [12]. In case of parasympathetic stimulation, less or no cortisol, hence vasodilation and blood pressure come down (Figure-2).
Basic functions of autonomic nervous system in IAYT: - a) Sympathetic (flight or fight response): Stress is part of our lives. Responses of stress includes 1) Stimulation of sympathetic nervous system which can increase blood pressure, heart rate, respiratory rate, 2) Blood glucose concentration in increased due to more secretion of cortisol which can increase blood glucose level, even more increase leads to hyperglycemia,3) Body immune system is inhibited due to hyperglycemia. Graphical representation (Figure-3) is given below. Subject has a chance to develop both hypertension and hyperglycaemia. These responses (flight & fight response) can be corrected after following IAYT [7].
b) Parasympathetic (rest& digest response): The parasympathetic nervous system is stimulated when one relaxes (Figure-4). Blood flow to the digestive system, brain, extremities & sexual organs is increased. metabolic activity in vascular tissues are adjusted, resulting blood pressure (BP), heart rate (HR) & respiratory rate are reduced or becomes normal (signs of improved parasympathetic tone). No sign and symptoms of both hypertension & hyperglycemia [7]. Subjects with all age groups feel joy, happiness, can decrease negative feeling of aggressiveness, depression and anxiety [7]. Yoga practices can increase multiple neurotransmitters and hormones such as GABA, serotonin & dopamine-all natural anti- depressants [7]. These neurotransmitters and hormones can increase the level of melatonin, helping to initiate sleep, improving sleep quality and also can help to secrete more oxytocin, the “bonding hormone”, thus helping with feeling of connectedness (Figure-4) [7].
c) Co-relation between the function of autonomic and various vascular cells in IAYT :-Endothelial dysfunction and autonomic nervous system dysfunction are both risk factors for atherosclerosis. There is evidence demonstrating that there is a close interrelationship between these two systems. In hypertension, endothelial dysfunction affects the pathologic process through autonomic nervous pathways, and the pathophysiological process of autonomic neuropathy in diabetes mellitus is closely related with vascular function [11-14]. However, detailed mechanisms of this interrelationship have not been clearly explained. In this review, we summarize findings concerning the interrelationship between vascular function and the autonomic nervous system may provide more comprehensive risk stratification and a new effective therapeutic strategy against atherosclerosis, hypertension and hyperglycemia [7,11-14]. Following important findings are noted. 1) Endothelial cell (EC) function is affected against ANS. Endothelial cells, vascular smooth muscle cells & nodal cells get hyperpolarized when there is a stimulation of PNS, resulting heart rate decreases, blood pressure goes normal, respiratory rate is also reduced.2) HPA axis is inhibited, less cortisol can reduce blood sugar level, hyperpolarization process in these vascular tissues will be operated, resulting normal arterial compliance. 3) More release of GABA, serotonin, dopamine, dehydroepiandrosterone (DHEA) can control emotion & behavior [7, 11-14]. 4) Less secretion of inflammatory markers would reduce inflammation. 5) Vascular function is nicely maintained, means process of contraction and relaxation of vascular smooth muscle, cardiac muscle would be proper with parasympathetic dominance (Figure-5).6) Telomerase enzymatic activity is increased which can protect cell deterioration and cell death (Figure-5). 7) Synaptic density and volume of prefrontal cortex, left hippocampus which can increase the long-term memory through increased release of neurotropic protein (BDNE). 8) Concentration of inflammatory markers is decreased, resulting no inflammation which again will help in maintaining blood pressure, atherosclerosis and hyperglycemia (7).

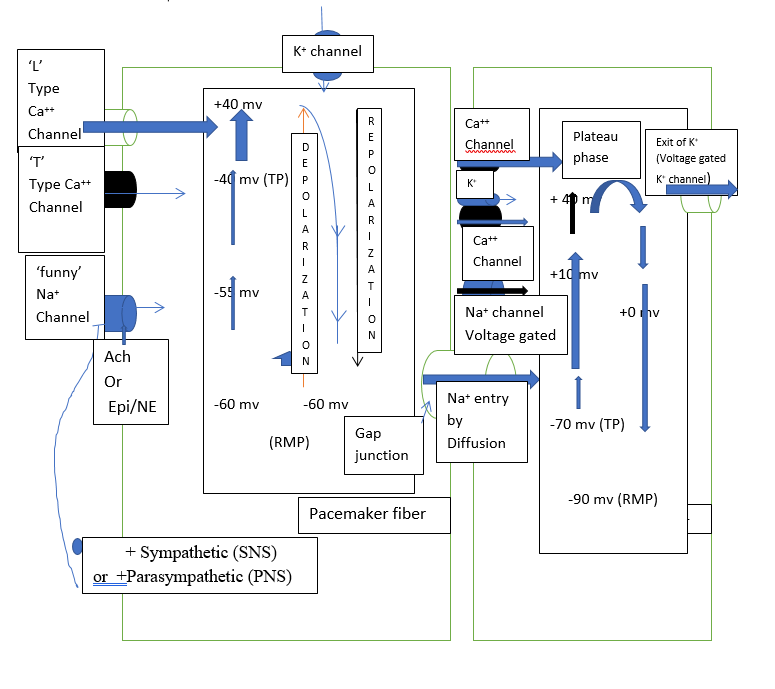
d) Basic molecular controlling mechanism of sympathetic (SNS) and parasympathetic (PNS)in vascular system: Resting Membrane Potential (RMP) in nodal fiber (pacemaker fiber) is -60 mv &-90 mv in contractile fiber in the heart (Figure-6). With the help of “funny Na+ channel”, ‘T’ type Ca++ channel and ‘L’ type Ca++ channel, K+ channel, electrical event goes on rhythmically, making nodal cell & contractile cell active till death. Some additional voltage gated Na+ channels are also operated in contractile cell to make resting membrane potential -90 mv during resting condition. Neurotransmitters like acetylcholine (Ach) or adrenaline/noradrenaline (Epi / NE) play an active role during the process of depolarization, repolarization and hyperpolarization expect only one plateau phase in contractile fiber present in heart. Hence, neuroendocrine process to IAYT cannot be overruled.
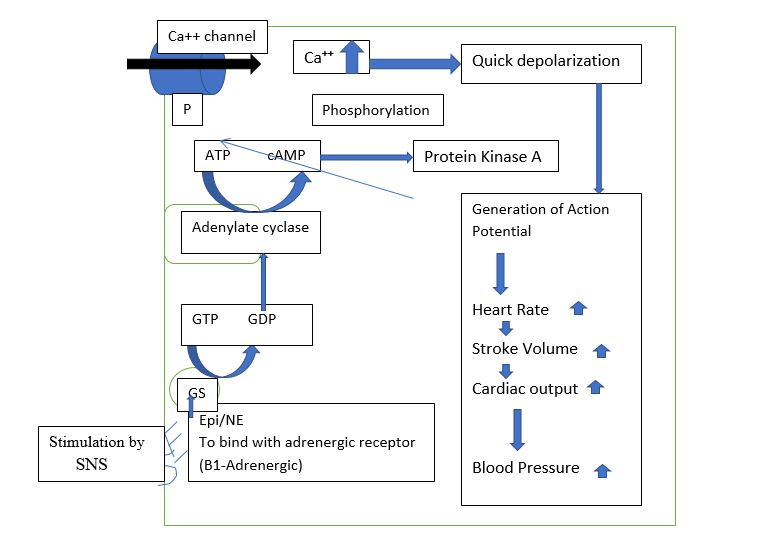
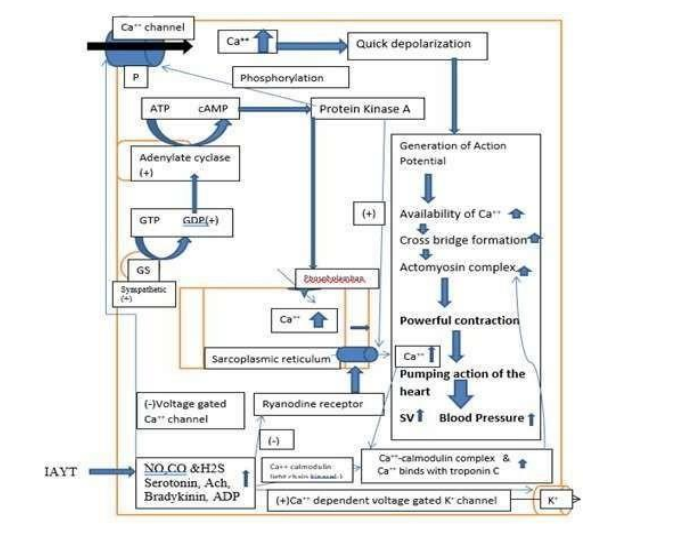
e) Responses from general basic extrinsic innervation of vascular system:- a)Sympathetic Nervous System (SNS)- In this, stimulatory G protein(GS) after binding with adrenergic neurotransmitter (Epi/NE) in the membrane can convert GTP to GDP as soon as adrenergic receptors are stimulated. GDP can form cAMP from ATP which actually stimulate protein kinase A. Protein kinase has a big role to stimulate voltage gated Ca++ channel, quick depolarization takes place. Cardiac output, stroke volume and heart rate are increased which can increase blood pressure (Figure-7).
f) Responses from general basic extrinsic innervation of parasympathetic only on nodal cell (pacemaker fiber):- Parasympathetic (vagal) activation, which releases acetylcholine onto the SA node that binds to muscarinic receptors having three units (α, β & ¥), decreases pacemaker rate by increasing potassium conductance and decreasing the pacemaker currents. Cyclic adenosine monophosphate (cAMP) is less produced due to stimulation of alpha unit of muscarinic M2 receptor (Figure-8).
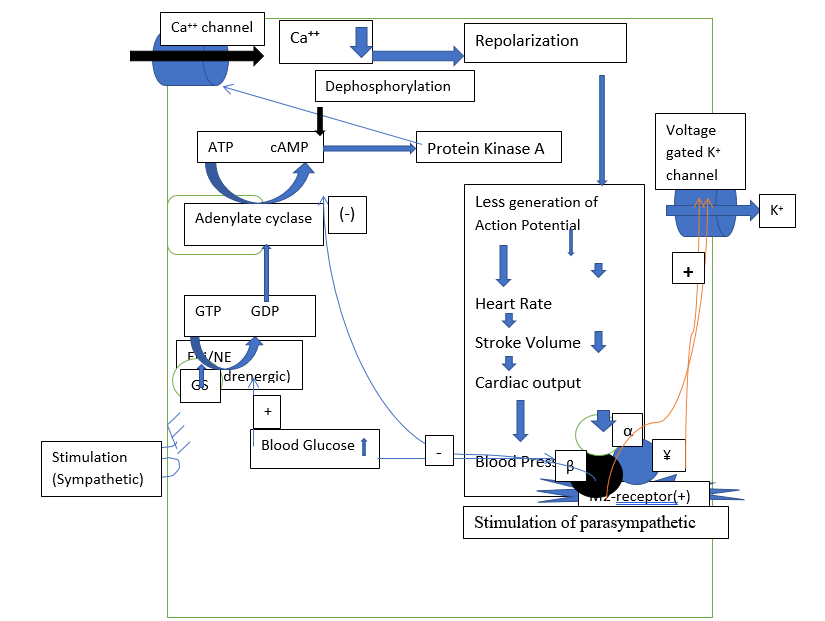
These changes in ion currents decrease the slope of phase 4 of the action potential, thereby increasing the time required to reach threshold. Voltage gated potassium channel is directly inhibited by β and ¥ unit of muscarinic receptor (Figure-8). Vagal activity also hyperpolarizes the pacemaker cell during Phase 4, which contributes to the longer time to reach threshold voltage. Heart rate & blood pressure are reduced.
g) Response of sympathetic on contractile cell & possible mechanism to IAYT: As per earlier sympathetic on contractile is stimulatory. Following IAYT, few important changes are noted. 1) Concentration of gaso transmitters (NO, CO, H2S) is increased (15-17), resulting inhibition of ryanodine receptors which actually reduce the transport of Ca++ from sarcoplasmic reticulum to cytosol, hence formation of Ca++ - calmodulin complexes. Less amount of formation of cross bridges takes place. Concentration of Ca++ in the contractile fiber decreases, but concentration in the sarcoplasmic reticulum is increased. 2) Concentration of serotonin, acetylcholine, bradykinin and ADP are increased, have inhibitory effect of ryanodine receptor, has an inhibitory effect on Ca++- calmodulin light chain kinase, resulting formation of less amount of Ca++ - calmodulin complex. 3)Gasotransmitter along with serotonin, bradykinin and ADP has a stimulatory effect of Ca++ dependent voltage gated K+ channel, and hence this is again inhibitory, allow fiber to relax (Figure-9)
Conclusions
World Health Organization (WHO) estimates that 80% of non-communicable diseases (NCD) deaths are due to four main diseases types: cardiovascular disease, cancer, diabetes and respiratory diseases. Unfortunately, lifestyle is the major causative factor on NCDs, including tobacco use, sedentary lifestyle, and lack of regular exercise, unhealthy diets and chronic psychological stress. Chronic inflammation and stress is a common factor of many of the NCDs, and an area where IAYT has been found to be extremely beneficial. IAYT can reduce stress with increased parasympathetic and reduced sympathetic activities respectively. Yoga practices (IAYT) can help to lower blood pressure, increase lung capacity, improve respiratory function and heart rate, improve circulation and boost muscle tone.
Acknoledgement
Author would like to thank his guide Dr Sohan Raj Tater as well as Dean of Singhania University for allowing him to work in the University. Author also conveys his thanks to all non - teaching staff to complete this work in the University.
References
- Prabu.P, et. al. Effect of Integrated Yoga Practice on Pancha Koshas (Five Sheaths) in healthy young adults-A Matched waitlist Control Trial. (2021). IOSR Journal of Dental and Medical Sciences (IOSR-JDMS); 20(02): 01-10.
- Susan J Zieman,Vojtech M and David AK. (2005).Mechanism,Pathophysiology and Therapy of Arterial Stiffness. Arteriosclerosis,Thrombosis and Vascular Biology. ; 25:932-943.
- Raub JA, (2002) Psychophysiologic effects of hatha yoga on musculoskeletal and cardiopulmonary function: A literature review. J Altern Complement Med; 8:797-812.
- M Jay Polsgrove BME.(2016). Impact of 10-weeks of yoga practice on flexibility and balance of college athletes. Int J Yoga. 2016;9(1):27–34.
- Cheema BS, Marshall PW, Chang D, Colagiuri B, Machliss B(2011). Effect of an office worksite-based yoga program on heart rate variability: A randomized controlled trial. BMC Public Health. BioMed Central Ltd; 11(1):578.
- Telles S, Yadav A KN(2013). Blood pressure and Purdue pegboard scores in individuals with hypertension after alternate nostril breathing, breath awareness, and no intervention intervention. Med Sci Monit. ;61–6.
- Stephens I,(2017) Medical Yoga Therapy.Children:4;12.
- Bhunia S, Tripathy N,(2013) A Comparative Analysis of Non-invasive Cardiovascular Functions in Proficient and Non-proficient Healthy Subjects. International Journal of Physiology 1(2):22-26.
- Snehasis Bhunia & Tater S.(2022) Effect of Integrated Approach of Yoga Therapy on Non-Invasive Cardiovascular Responses: Study on Young and Older Healthy Males. Asian Journal of Research in Cardiovascular Diseases. 4(4): 39-47.
- Woodyard C, (2011). Exploring the therapeutic effects of yoga and its ability to increase quality of life International Journal of Yoga ;4(2):49-54
- Najeeb A Shirwany, Ming-hui Zou. (2010) Arterial stiffness: a brief review. Acta Phyarmacologica Sinica;31:1267-1276
- Boyang Lv,Selena Chen, Choshu T,Hongfang Jin, Junbao Du, Yaquin Huang.(2021) Hydrogen sulphide and vascular regulation-An update. Journal of Advanced Research; 27: 85-97.
- Alicia Saz-Lara, Iván Cavero-Redondo, Celia Álvarez-Bueno, Blanca Notario-Pacheco,Marta Carolina Ruiz-Grao and Vicente Martínez-Vizcaíno, (2021).The Acute Effect of Exercise on Arterial Stiffness in Healthy Subjects: A Meta- Analaysis J. Clin. Med.; 10, 291
- Valentina Citi, Alma Martelli, Era Gorica, Simone Brogi, Lara Testai, Vincenzo Calderone Role of hydrogen sulfide in endothelial dysfunction: Pathophysiology and therapeutic approaches Journal of Advanced Research. 27: 99-113.
- Richard C Jin, Joseph Loscalzo (2010). Vascular nitric oxide: formation & function Journal of Blood Medicine; 1:147-162.
- Snehasis Bhunia (2002). A Physiologist’s view on Yoga. Yoga and Total Health, July 2002; XL VII (12): 8-9.
- Snehasis Bhunia (2010). Can physical exercise, control on diet and naturopathic treatment prevent early development of diabetes mellitus? Indian Journal Physiol Pharmacol ;54(1):92-94.


