Archive : Article / Volume 2, Issue 2
- Research Article | DOI:
- https://doi.org/10.58489/2836-5917/010
The Overestimation of Heart Failure in Cause-of-Death Statistics
1 Statistics Netherlands (CBS), Cause-of-death statistics, The Netherlands.
P.P.M. Harteloh
P.P.M. Harteloh (2023), The Overestimation of Heart Failure in Cause-of-Death Statistics, Clinical Cardiovascular Research.2(2). DOI: 10.58489/2836-5917/010
© 2023 P.P.M. Harteloh, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 01-02-2023
- Accepted Date: 23-02-2023
- Published Date: 18-05-2023
heart failure; underlying cause of death; cause-of-death statistics; death certificate; mortality statistics
Abstract
Heart Failure is one of the top ten leading causes of death in mortality statistics. Mortality statistics report underlying causes of death, i.e. starting points of causal chains leading to death. Heart failure always has a cause and therefore cannot be such a starting point. Therefore, the aim of this study is to explain the occurrence of heart failure in mortality statistics. Survey among a sample of 750 certifiers who mentioned heart failure on a death certificate. Comparison of the physician's opinion on the role of heart failure as a cause of death with the outcome of automated coding for statistics. The survey response was 56%. When a doctor mentions heart failure on a death certificate, the disease is considered underlying cause of death in 21.4% of the cases. In statistics, the disease is assigned this role in 39.2% of the (same) cases. Heart failure is overestimated by 17.8 percentage points or 45% (95%-CI: 40-50%) in mortality statistics. In cause-of-death statistics, heart failure is more often regarded as underlying cause of death than intended by the certifying physician. This overestimation is caused by incorrectly completed death certificates, conceptual confusion and a real difference in opinion on the role of heart failure as underlying cause of death.
Method
A questionnaire was designed to investigate the role of heart failure as a cause of death. Based on literature and medical guidelines, statements were included about the causal role of heart failure in dying. A draft of the questionnaire has been submitted to five expert clinicians and, after processing their comments and suggestions, has been tested by a number of doctors in the field. The final questionnaire was sent to 750 doctors who reported heart failure as a cause of death on a death certificate in 2017 (regular year: no influenza or COVID-19 epidemic). This was a random sample from the collection of all death certificates mentioning heart failure, regardless of whether or not this disease was selected as the underlying cause of death for statistics. A distinction was made between death certificates only mention heart failure (approximately 20%) - whereby no other underlying cause of death could be selected than heart failure - and death certificates containing other causes of death in addition to heart failure (approximately 80%). The sample frame contained nearly 25,000 death certificates mentioning heart failure. The sample contained 44 deceased men and 56deceased women with an average age at death of 81.6 and 86.0 years, respectively. The questionnaire was accompanied by the death certificate completed by the certifying doctor himself.
Of the doctors addressed, almost 56% returned a completed questionnaire (n=419). The majority of respondents were General Practitioners (48%). More than 32 were specialists elderly medicine and nearly 20 belonged to a hospital- related specialism. Almost 17% of the doctors approached were no longer available at the address stated on the death certificate. They had changed job or work location. About 5% of the doctors approached indicated that they did not want to or could not complete the questionnaire. They stated the medical record of the deceased was no longer available to them and/or they did not remember the particular case well enough. Of almost 23 of the doctors approached, nothing was heard even after a reminder (Table 1). Of the doctors who completed the questionnaire, 82 had more than 2 years of work experience. More than 41% of the respondents filled out a death certificate 6-15 times a year, 23 did so 16-25 times and 26% even more than 26 times a year. The majority of respondents therefore have extensive experience in completing death certificates.
Death certificates of the respondents had been coded separately from this research by Statistics Netherlands for the regular production of cause-of-death statistics. Coding was done automatically by the Iris computer program, version 4.4.1, including the international (WHO) guidelines for coding and selecting an underlying cause of death and the ICD-10 updates of 2017. [8-10].
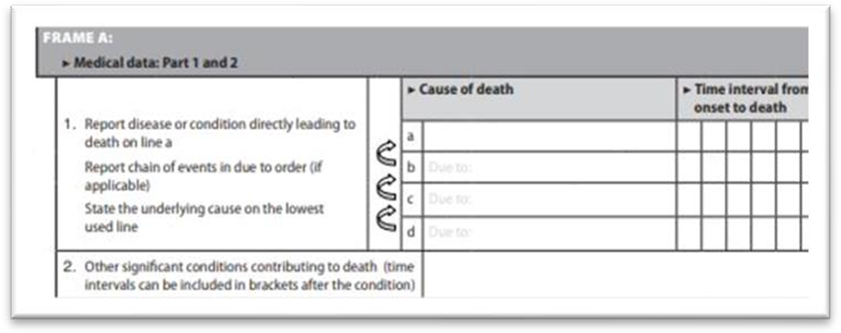
For evaluating completed death certificates, the WHO format for reporting causes of death was used (box 1). In the Netherlands, part 1 is restricted to the lines 1a-1c, so that the underlying cause of death is expected to be written on line 1b or line 1c. Causes of death are described in plain medical terminology. They are coded by medical coders of Statistics Netherlands, not by the certifier [10].
| Number | % |
Respondents who filled in the questionnaire | 419 | 55.9 |
Respondents who refused to fill in the questionnaire | 34 | 4.5 |
Doctors not at address as stated on the death certificate | 127 | 16.9 |
Non response (no reaction) | 170 | 22.7 |
Medical specialism of respondent (n = 419) |
|
|
General Practice (GP) | 201 | 48.0 |
Specialist Elderly Medicine | 136 | 32.5 |
Geriatric medicine | 7 | 1.7 |
Internal medicine | 15 | 3.6 |
Cardiology | 17 | 4.1 |
Other (e.g., IC or Acute medicine) | 43 | 10.3 |
Table 1. Response of survey (n = 750) | ||
Results
When a doctor mentions heart failure on a death certificate, the disease is considered the underlying cause of death in 21.4% of the cases. In 31.7% of the cases, the doctor considers heart failure a direct cause of death; in 35.9% of the cases a contributing cause of death, and in 5.7% of the cases the doctor indicates that heart failure, despite mentioning it on the death certificate, did not play a role in dying at all. The heart failure was just present at the time of death. With automated coding for cause-of-death statistics, the disease is the underlying cause of death in 39.2% of the (same) cases. Almost half of these cases are from death certificates with only heart failure as tcause of death. With regard to the opinion of the certifying doctor, heart failure is overestimated as the underlying cause of death by 17.8 percentage points or 45% (95%-CI: 40-50%) in mortality statistics (Table 2).
According to the (WHO) principle of selecting an underlying cause of death, heart failure should be coded by its cause. However, our survey showed that the cause of heart failure was not known to 45% of the doctors who completed the death certificate. These certifiers could report heart failure as a cause of death, but not its cause (knowledge gap). On the other hand, in case Iris did select heart failure for cause-of-death statistics as the underlying cause of death, the cause of heart failure was known to the doctor who completed the death certificate in almost 50% of the cases. When certifiers had reported this cause, Iris would not have selected heart failure as the underlying cause of death for mortality statistics (reporting error).
When asked whether the person would have died if he or she had not suffered from heart failure (counterfactual),[11] 40% of the respondents answered: “(probably) yes”. Heart failure does not play a causal role in the event of death and should not have been reported on the death certificate (insufficient causal reasoning). This percentage was 51% for the specialist’s elderly medicine, 47% for the medical specialist, and 28% for the general practitioner.
If death certificates (i) mention only heart failure and no other cause of death, (ii) with a positive response to the counterfactual (person died regardless of the heart failure), or (iii) with a known cause of heart failure are excluded because heart failure should not be considered the underlying cause of death in these cases, 68 records remain, with Iris selecting heart failure as the underlying cause of death in 23 cases (34%) and the doctor doing so in 18 cases (27%) (coding/selection error).
Position of heart failure on death certificate | Role of heartfailure as the Cause of Death |
Total | |||||||
According to certifier | According to Iris/CoD Statistics | ||||||||
| Direct CoD | Intermediate CoD | Underlying CoD |
Contributory CoD |
Not a CoD |
Underlying CoD | No underlying CoD |
| ||
Part 1a. (single entry)** |
| 51 | 0 | 24 | 3 | 0 | 78 | 0 | 78 |
% row | 65.4% | 0.0% | 30.8% | 3.8% | 0.0% | 100.0% | 0.0% | 100.0% | |
% column | 40.2% | 0.0% | 27.9% | 2.1% | 0.0% | 49.7% | 0.0% | 19.5% | |
Part 1a. (more than one entry)*** |
| 47 | 7 | 15 | 12 | 0 | 20 | 61 | 81 |
% row | 58.0% | 8.6% | 18.5% | 14.8% | 0.0% | 24.7% | 75.3% | 100.0% | |
% column | 37.0% | 33.3% | 17.4% | 8.3% | 0.0% | 12.7% | 25.0% | 20.2% | |
Part 1b |
| 16 | 7 | 24 | 26 | 0 | 25 | 48 | 73 |
% row | 21.9% | 9.6% | 32.9% | 35.6% | 0.0% | 34.2% | 65.8% | 100.0% | |
% column | 12.6% | 33.3% | 27.9% | 18.1% | 0.0% | 15.9% | 19.7% | 18.2% | |
Part 1c |
| 11 | 5 | 22 | 43 | 4 | 31 | 54 | 85 |
% row | 12.9% | 5.9% | 25.9% | 50.6% | 4.7% | 36.5% | 63.5% | 100.0% | |
% column | 8.7% | 23.8% | 25.6% | 29.9% | 17.4% | 19.7% | 22.1% | 21.2% | |
Part 2 |
| 2 | 2 | 1 | 60 | 19 | 4 | 80 | 84 |
% row | 2.4% | 2.4% | 1.2% | 71.1% | 22.9% | 3.6% | 96.4% | 100.0% | |
% column | 1.6% | 9.5% | 1.2% | 41.7% | 82.6% | 1.9% | 32.8% | 20.9% | |
Total |
| 127 | 21 | 86 | 144 | 23 | 157 | 244 | 401 |
|
|
|
|
|
|
|
|
| |
% row | 31.7% | 5.2% | 21.4% | 35.9% | 5.7% | 39.2% | 60.8% | 100.0% | |
Table 2. The role of heart failure as the cause of death according to the doctor who completed the death certificate and according to the Iris software for automated coding of causes of death (n = 419) *
*Light gray = position on the death certificate in accordance with role as a cause of death. Dark gray = heart failure should not have been reported as a cause of death; CoD = Cause of Death; Part 1a: position of direct CoD; Part 1b: position of intermediate CoD (if any); Part 1b or part 1c: position of underlying CoD (lowest line used); part 2: position of contributory CoD (see: box 1).
** Death certificates with heart failure as the only cause of death (n= 78)
*** Death certificates with heart failure in part 1a and other CoD (n=81)
Discussion
This study. The physician's assessment of the role of heart failure as a cause of death was studied. Inquiries were made about the background of completed death certificates. The intention of the certifier was compared with the outcome of coding for cause-of-death statistics. The study is an evaluation of the coding process. It is an addition to studies evaluating the certification process by comparing a completed death certificate with the medical record or autopsy of the deceased. [4-7][11]
The strong points of this research are furthermore the good response, the educational nature when it comes to completing a death certificate, and the direct link with cause-of-death statistics. The limitation is the lack of (additional) qualitative research to better understand the observed difference between the formal (WHO) definitions and the way certifying doctors use the corresponding concepts.
*Light gray = position on the death certificate in accordance with role as a cause of death. Dark gray = heart failure should not have been reported as a cause of death; CoD = Cause of Death; Part 1a: position of direct CoD; Part 1b: position of intermediate CoD (if any); Part 1b or part 1c: position of underlying CoD (lowest line used); part 2: position of contributory CoD (see: box 1).
** Death certificates with heart failure as the only cause of death (n= 78)
*** Death certificates with heart failure in part 1a and other CoD (n=81)
Interpretation of the results. The (WHO) definition of "underlying cause of death" requires the coding of a disorder or disease by its cause.[1] Since heart failure is always the result of another disease or condition, it cannot actually be qualified as the underlying cause of death. The frequent occurrence of heart failure in cause-of-death statistics (annual prevalence = approximately 5%) therefore requires explanations. This study identifies several:
1. Knowledge gap and reporting errors. The certifying physician does not always know or does not always report the cause of heart failure on the death certificate. It appears that the cause of the heart failure is often (45%) unknown to the certifier. This may be due to a lack of knowledge of the (complete) disease history of the patient, for instance when the death certificate is completed on-site in the absence of the medical record or the cause of heart failure (like a rheumatic valve disease) lies in a distant past. If the certifying physician knows the cause of the heart failure, a lack of knowledge of the WHO principles for selecting the underlying cause of death may also hinder a proper reporting of heart failure on a death certificate.
2. (In)correctly filled in the death certificate. As Table 2 shows, the position of heart failure on the death certificate does not always correspond to the role that the doctor assigns the disease in the event of death.
WHO defines the format of a death certificate and the rules for reporting an underlying cause of death in the instruction manual of the ICD-10.[1] According to the ICD-10 instruction manual, this underlying cause of death is expected on the lowest-used line of part 1 of the death certificate (part 1b or part 1c) (see: box 1). However, 45.3% (table 2: 27.9+17.4%) of the certifiers who consider heart failure the underlying cause of death, noted heart failure on part 1a of the death certificate, i.e., the place of a direct cause of death.
Also, in more than a third of the cases (35.9%) certifiers considered heart failure a contributing cause, that is, the patient dies of another disease because he or she also had heart failure. Heart failure is then a sufficient, but not necessary condition for death. [12-13]. When the doctor considers heart failure a contributing cause of death, in 41.7% of the cases it is (correctly) noted on part 2 of the death certificate, in 58.3%. Certifiers considered heart failure a direct cause of death in 31.7% of the deaths. In 77.2% (table 2: 40.2+37.0%) of such cases, heart failure is correctly noted in part 1a of the death certificate. However, 21.3% (table 2: 12.6+8.7%) of the certifiers who consider heart failure a direct cause of death noted heart failure on part 1b or 1c of the death certificate, whereby it can be no direct cause of death since something - stated on 1a - must have been in between heart failure and death.
In 65.4% of the death certificates with only heart failure noted at position 1a, the certifier left out the underlying cause of death (incomplete death certificates). In 30.8% of these cases, heart failure is said to be the underlying cause of death and thus incorrectly noted at position 1a of the death certificate (reporting error).
When death certificates with only heart failure are not taken into consideration, then according to the intention of the certifying physician heart failure is noted on the correct position of the death certificate in 50% of the cases (light gray fields in Table 2: 160/323). In literature, estimates of accuracy vary from 40-60% of the death certificates completed correctly.[11] [14-15] The finding of this study is in line with these estimates.
3. Conceptual difference. The certifying doctor has a different opinion on the underlying cause of death than the formal definition WHO prescribes.
Given the (correct) position on the death certificate (line 1b or 1c), in 11% (table 2: 46/401) of the cases, the physician actually considers heart failure the underlying cause of death. An example of this is a long-term, progressively worsening chronic heart failure with a cause in the distant past (for example, rheumatic valve disease in early childhood). In such a case, chronic heart failure dominates the patient's suffering, leading to a cardiac output incompatible with life. In fact, the underlying disease is considered equal to the underlying cause of death. Thus, the certifier gives "underlying” a different meaning than the WHO, which asks a doctor to report the beginning of a causal chain.
4. Automated coding. With automated coding, the Iris software considers heart failure (much) more often as the underlying cause of death than the doctor would do. Given the doctor’s opinion, the software overestimates heart failure as a cause of death by 45%. A large part of this overestimation is caused by death certificates on which only heart failure is stated and no other causes of death (n=78). In these cases, the software cannot actually make a choice. If we do not consider death certificates with heart failure as the only cause of death, the difference between the doctor's opinion on the underlying cause of death and the result of automated coding is still 5.4 percentage points or 21.5% (table 2: 62/323 versus 79/323). Thus, the Iris software is responsible for about half of the overestimation in mortality statistics.
5. Causal reasoning. About 40% of the respondents indicate that the patient would have died if they would not have heart failure at the time of death (counterfactual). In such cases, the doctor notes heart failure present at the time of death on the death certificate, while it does not play a causal role in the event of death at all. A death certificate is not intended to register diseases or disorders present at the time of death, but should (only) report diseases or disorders playing a role in the causal mechanisms of death.[16] As heart failure is often present at the time of death (prevalence: 8-20%),[3] the certifier should evaluate its role as a cause of death more carefully. This requires practice in causal reasoning, i.e. application of the counterfactual when completing the death certificate.[11] [14]
Conclusion
In the cause-of-death statistics, heart failure is more often regarded as the underlying cause of death than the certifying physician would do. With respect to the certifier’s opinion, the overestimation in mortality statistics is 45% (95%-CI: 40- 50%). This overestimation is based on incorrectly or incompletely filled-in death certificates, conceptual confusion, and a real difference in opinion on the role of heart failure as the underlying cause of death.
Number of words: 2443
Disclosure: The author had nothing to disclose
Funding: There was no additional funding
Disclaimer: The views expressed in this article are solely those of the author and do not necessarily comply with the views or policy of Statistics Netherlands
Introduction
With nearly 25,000 entries per year, heart failure is one of the most common causes of death reported on death certificates in the Netherlands. From these entries, the so-called underlying cause of death - defined as the disease or disorder that has triggered the causal series of events that led directly to death is selected for cause-of-death statistics as prescribed by the ICD-10 instruction manual.[1] The result is about 5% of the deceased dying from heart failure (ICD-10 code I50) each year and a ranking of heart failure in the top ten of the most common underlying causes of death.[2] However, as heart failure is always the result of another disease (myocardial infarction, cardiomyopathy, heart valve disease, COPD or hypertension),[3] death should be assigned to its cause and heart failure can actually never be underlying cause of death. So, how can the occurrence of heart failure in cause-of-death statistics be explained? Research on death certificates mentioning heart failure was carried out in order to answer this question. Often, this is done by comparing a completed death certificate with the medical record (including the patient’s history) or autopsy of the deceased. [4-7] This study takes a different approach. Certifiers were questioned about the role they assigned heart failure as cause of death. Subsequently, the opinion of the certifier was compared with the actual coding of heart failure as underlying cause of death for mortality statistics. The study can be considered an evaluation of the coding process. It is not an evaluation of the certification process by a golden standard (medical history or autopsy).
References
- WHO. World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Volume 2 (Instruction manual). Geneva: WHO, 2016.
- CBS (Centraal Bureau voor de Statistiek)
- Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007; 93: 1137-46
- Stevens GA, King G, Shibuya K. (2010) Deaths from heart cause-of-death
- Johansson LA, Westerling R. (2002) Comparing hospital discharge records with death certificates: can the differences be explained? J Epidemiol Community Health; 56:301-8.
- Maclaine GD, Macarthur EB, Heathcote CR. (1992) A comparison of death certificates and autopsies in the Australian Capital Territory. Med J Aust.; 156:462-3, 466-8.
- Ravakhah K: (2006) Death certificates are not reliable: revivification of the autopsy. South Med J; 99:728-733.
- Iris Institute (2023):
- World Health Organization (WHO). List of Official ICD-10 Updates.
- Harteloh P. (2018) The implementation of an automated coding system for cause-of-death statistics. Informatics for Health and Social Care; 45: 1-14.
- Schuppener LM, Olson K, Brooks EG. (2020) Death Certification: Errors and Interventions. Clin Med Res.; 18:21- 26.
- Araújo de LFSC, Dalgalarrondo P, Banzato CEM. On the notion of causality in medicine: addressing Austin Bradford Hill and John L. Mackie. (2014) Archives of Clinical Psychiatry; 41:56-61.
- Vineis P. (2003) Causality in epidemiology. Sozial-und Präventivmedizin; 48: 80-7.
- Carter E, Holt C, Haskins A. (2017) Death Certificate Accuracy — Why It Matters and How to Achieve It. Today's Geriatric Medicine;10:26.
- Selinger CP1, Ellis RA, Harrington MG. (2007) A good death certificate: improved performance by simple educational measures. Postgrad Med J.;83:285-286.
- Kotabagi RB, Chaturvedi RK, Banerjee A. (2004) Medical Certification of Cause of Death. Med J Armed Forces India;60


