Archive : Article / Volume 2, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-5917/005
Incidental Coronary Artery Disease on Routine CT Coronary Angiography âAn evidence-based approach
- Senior Consultant Cardiologist National Heart Institute,49-50, Community Centre East of Kailash New Delhi â 110 065.
- PG Resident, HIMSR, Jamia Hamdard, Unit, New Delhi.
Vinod Sharma
V. Sharma, R. Sharma (2023). Incidental Coronary Artery Disease on Routine CT Coronary Angiography âAn evidence-based approachâ. Clinical Cardiovascular Research. 2(1). DOI 10.58489/2836-5917/005
© 2023Vinod Sharma, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 19-12-2022
- Accepted Date: 04-01-2023
- Published Date: 16-01-2023
Abstract
Introduction
Atherosclerotic coronary artery disease is the leading cause of high morbidity and mortality across the globe [1]. Coronary CT angiography has emerged as a highly accurate non-invasive diagnostic modality for the diagnosis of atherosclerotic coronary artery disease [2]. Coronary CT angiography should be considered as an alternative to stress imaging technique for ruling out atherosclerotic coronary artery disease in patients with the lower range of intermediate pre-test probability for atherosclerotic stable coronary artery disease. However, coronary CT angiography is not recommended as a screening test in asymptomatic individuals without clinical suspicion of coronary artery disease. CT Coronary angiography has been performed routinely before many of the cardiac and non-cardiac procedures like TAVI, atrial fibrillation ablation prior to the organ transplantation. Many a times, advised by Family Physician or patients themselves for a routine screening for atherosclerotic coronary artery disease undergo CT coronary angiography. When incidental atherosclerotic coronary artery disease is found in such patients who do not have any typical or atypical symptom suggestive of coronary artery disease then question arises how to approach this patient as far as the risk estimation for future adverse cardiovascular event and prognostication is concerned. It also becomes imperative to decide the line of management for this patient. To answer these two pertinent questions, we need to understand the behavior and natural history of atherosclerosis & performance of CT coronary angiography in diagnosis and in predicting the prognosis of atherosclerotic disease.
Performance of CT Coronary Angiography: -
Atherosclerosis is usually generalized rather than a focal process. It is dynamic in nature with atherosclerotic plaque undergoing biological remodeling and compositional alteration time to time. It is process in continuum and displays phases of stability and instability. Coronary stenosis resulting from atherosclerosis is a powerful although debated prognostic indicator of CAD as far as the clinical outcome is concerned. Morphology, composition and degree of inflammation of coronary atherosclerotic plaque are more important than the degree of luminal stenosis. The consequence of plaque composition leading to acute coronary syndrome depends not only on the composition of atheroma itself but many other factors like local rheological and hemodynamic phenomenon which determines the rupture of plaque. More than 2/3rd of acute MI occurs in a non-obstructive atheromatous lesion. CT coronary angiography is an excellent imaging technique for both quantitating atherosclerotic burden and obtaining qualitative information regarding plaque composition [2]. It offers non-invasive visualization and better mapping of atherosclerosis akeen to the ophthalmoscope. CT angio gives information derived by both invasive coronary angiography and intravascular ultrasound by showing the lumen as well as imaging the vessel wall. CT coronary angiography has a high sensitivity 98% and specificity 98% with a negative predictive value of 95 – 100% to rule out obstructive coronary artery diseas[3]. CT angiography besides defining the extent and severity of coronary artery stenosis also gives a fair amount of idea about plaque morphology (whether it is calcified, mixed or non-calcified). It does help in sub-classification of plaque component and therefore it helps in defining prognosis in case of low to moderate risk subjects and also helps in therapeutic intervention guidance. As a whole CT coronary angiography appears to be a tool for personalized risk prediction and individualized medical therapy.
Prognostic Significance of Atherosclerotic CAD: -
Finding of obstructive CAD in coronary CTA is associated with significant (6- to 12- fold) increase in the risk of future cardiovascular events, independent of traditional cardiovascular risk factors [4]. In addition, the absence of CAD carries a nearly perfect negative predictive value ( 99%). The detection of non-obstructive CAD defined as coronary atherosclerosis causing luminal narrowing between 1% & 69% has come out as a significant and frequent finding. Though it may not be associated with reversible myocardial ischemia but carries a substantial risk for future major adverse cardiovascular events (MACE) in comparison to the patients who do not have evidence of any atherosclerosis in CT Angio [5].
Several studies have demonstrated the prognostic significance of atherosclerotic lesion demonstrated in CT Coronary angiography.
- The multi-center CONFIRM study concluded that the anatomical stenosis severity of coronary artery disease was associated with higher mortality rate [6]. 23,854 patients without known coronary artery disease were enrolled in this study. They observed that patients with non-obstructive (less than 50%) and obstructive CAD (more than 50%) had 1.6 and 2.6-fold higher mortality risk compared to those with normal coronary artery. Besides the stenosis severity, the extent of coronary stenosis in one vessel (HR 2.00, 95% CI 1.43 – 2.82, p Value less than 0.0001), two vessel disease (HR 2.92, 95% CI 2.00 – 4.25, p value less than 0.0001), and triple vessel disease or left main disease (HR 3.70, 95% CI 2.58 – 5.29, p value less than 0.0001) were associated with higher mortality risk. The mortality risk was seen not only with obstructive stenosis with more than 50%, but also with non-obstructive stenosis with less than 50%.
- In the CONFIRM Registry the prevalence of obstructive CAD in 7,590 asymptomatic patients was 25% with a 1.6% annual mortality rate compared with 0.7% events per year in patients with no obstructive CAD. More importantly multi-vessel CAD (2 or 3 vessel / left main) was associated with a higher mortality compared with patients without CAD.
- Cheruvu & Colleagues studied [7]1,884 patients without prior CAD or any modifiable CAD risk factors. Among this low-risk group (mean age 55.6 years) followed for a mean of 5.6 + 1.3 years, the presence of more than 1 segment of non-obstructive CAD (HR 1.73, 1.08 – 2.71), obstructive (more than 50%), one or two vessel disease (HR 1.7, 1.08 – 2.71) and three vessel or left main obstructive CAD (HR 2.87, 1.57 – 5.23) were significantly associated with increase in all-cause mortality.
Similarly, the incidence of MACE (all cause death, non-fatal MI, unstable angina or late coronary revascularization) increased from 5.6% in those without CAD to 13.24% in those with non-obstructive disease and to 36.28% in those with obstructive CAD (p 0.0001). These results highlight the prognostic implication of manifest CAD on coronary CTA among patients without cardiovascular risk factors, and the potential of these findings to refine management.
- Lin et al [8] in their study of “mortality risk in symptomatic patients with non-obstructive coronary artery disease” of 2583 patients showed that the presence and extent of non-obstructive CAD were associated with worsening mortality during 3.1 + 0.5 years.
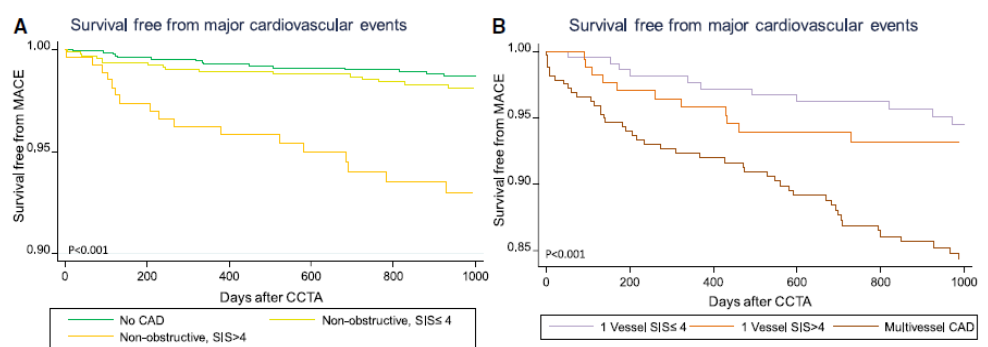
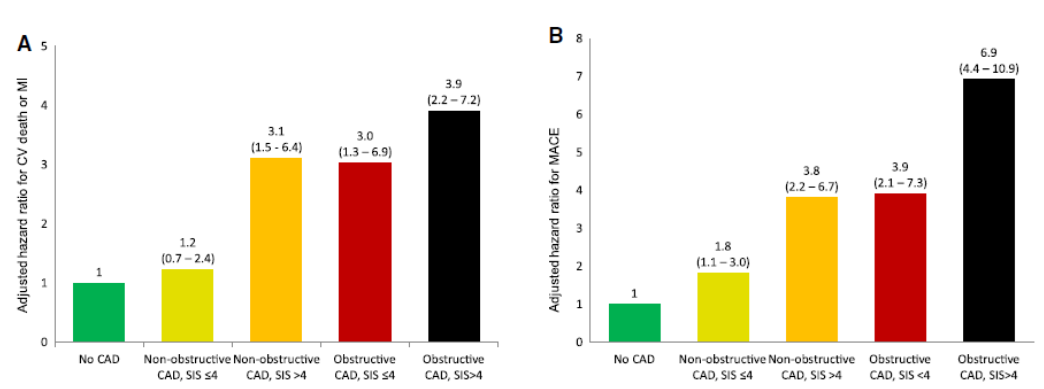
- Bittencourt et al[9] study of prognostic value of non-obstructive and obstructive coronary artery disease & non-extensive (less than 4 segments) and extensive (more than 4 segments) CAD revealed in their study of 3,032 patients, who were followed for a median of 3.6 years observed that extensive obstructive CAD (HR 3.9, 95% CI 2.2 – 7.2), extensive non obstructive CAD (HR 3.1, 95% CI, 1.5 – 6.4) and non-extensive obstructive CAD (HR 3, 95% CI, 1.3 – 6.9) were associated with the increase cardiovascular events including cardiovascular death or myocardial infarction. In this study, they found that subjects with extensive non-obstructive CAD experienced greater risk compared to those with non-extensive obstructive CAD.
- Blanke & others [10] compared outcomes between 1823 patients with diabetes to 1823 propensity matched patients without diabetes who were followed for 5 years following coronary CT angiography for incident mortality. They found that patients with diabetes did not exhibit an increased risk of mortality compared with the propensity matched non-diabetic subjects in the absence of CAD (HR 1.32, 0.78 – 2.24; p = 0.296). However, among subjects with non-obstructive CAD on CT angiography, diabetic patients were at significantly increased risk of death (HR 2.10; 1.43 – 3.09) with a mortality risk that was higher than non-diabetic patients with obstructive ( 50% stenosis) CAD. These data highlight the clinical implication of coronary artery disease both obstructive and non-obstructive in diabetic patients.
Analyzing the all-cause mortality benefit of coronary revascularization versus medical therapy in patients without known coronary artery disease undergoing coronary computed tomography angiography, Min et al [11] from the CONFIRM trial investigated 15,223 patients without known coronary artery disease by performing CT angiography. High risk CAD incorporating left main disease, more than 50% stenosis, more than 3 segments with more than 70% stenosis or more than 2 segments with more than 70% stenosis, and the proximal LAD with more than 70% stenosis was associated with the benefit of revascularization compared to non-high-risk CAD.
The atherosclerosis develops stepwise in stages. Rupture prone vulnerable plaque with a large necrotic core and thin fibrous cap containing many inflammatory cells such as macrophages and characterized by positive remodeling, develops at a relatively early stage. In particular, positive remodeling refers to compensatory enlargement of the vessel diameter to maintain the lumen develops during the early stage of plaque progression. Because extensive calcification appears at the late stage of atherosclerotic progression, the prevalence of high-risk plaque characterized by positive remodeling, low density plaque and none or spotty calcification could decrease in extensive calcified lesion, such as those with Agatston score of more than 500.
CT Coronary angiography has capability of visualization of coronary plaque type and / or vulnerability associated with plaque rupture beyond stenosis. The coronary plaque with vulnerability feature is so called “vulnerable plaque”. These adverse plaques are more likely to contain large necrotic cores, a thin cap fibroatheroma (TCFA), positive arterial remodeling, and / or spotty calcification. All these compositional features are associated with heighten cardiovascular events. The finding of vulnerable plaque on CCTA are represented by low attenuation plaque (LAP), positive remodeling or spotty calcification.
Bourantas et al [12] examined the relationship between clinical and angiographic characteristics to high-risk plaque defined as plaque with more than 2 high risk features including TCFA, plaque burden more than 70% and / or minimal luminal area less than 4 mm2 detected by IVUS. Compared to subjects with low-risk plaque, they observed that dose with high-risk plaque experienced higher cardiovascular risk (HR 2.63; 95% CI, 1.62 – 4.26; p less than 0.001).
Motoyama & colleagues[13,14] followed 1,059 patients with non-obstructive CAD on coronary CT angio over a mean of 27 months. Within this cohort, the presence of CAD with both positive [expensile remodeling (PR)] and low attenuation plaque (LAP), defined as any plaque component less than 30% Hounsfield units (HU) was associated with more than a 20-fold increase likelihood of subsequent acute coronary syndrome (ACS) (HR 22.8, 6.9 – 75.2). Beside this, coronary plaque that were shown to be culprit lesion in future ACS events were noted to have increased remodeling index (RI 1.27 Vs 1.13, p = 0.003), total plaque volume (134.9 Vs 57.58 mm 3, p less than 0.001) and LAP volume (20.4 Vs 1.1mm3, p less than 0.001). The high risk or vulnerable plaque characteristic implies increased risk of MACE. Findings of spotty calcification (less than 3 mm diameter), increased lesion length, total coronary plaque burden and the presence of napkin ring sign (NRS), generally defined as peripheral plaque enhancement surrounding lower attenuation plaque.
Ahmadi et al [15], examined 1102 symptomatic subjects with non-obstructive coronary artery disease detected by Electron Beam CT and demonstrated that non obstructive non calcified plaque (NCP) or partially calcified plaque (PCP) inclusive of both non calcified and calcified plaque components, as compared to calcified plaque (CP) alone imparted a higher prevalence of long term adverse clinical outcomes in a follow up of 78 + 12 months. Subjects with NCP experienced 7 folds higher incident mortality compared to those with CP (96% Vs 1.4%) and 3 folds higher than those with PCP (9.6% Vs 3.3%).
To understand the potential impact of plaque morphology on prognosis, Feuchtner & colleague[16] evaluated 1,469 low to intermediate risk patients with coronary CTA for stenosis severity (minimal less than 10%, mild less than 50%, moderate 50 – 70%, severe more than 70%), plaque type (calcified, mixed dominantly calcified, mixed dominantly non-calcified, non-calcified) and high-risk plaque criteria (LAP, NRS, spotty calcification less than 3 mm and RI). Over a follow up of 7.8 years, the presence of LAP (less than 60 HU), and NRS were the strongest predictors of incident MACE (adjusted HR 4.96 and 3.85, respectively, p value less than 0.0001) with stenosis more than 50% (HR 1.5, 1.1 – 2.3) and increased non-calcified plaque component (HR 1.7, 1.1 – 2.6) also predictive in adjusted models.
Nadjiri et al[17] followed 1,168 consecutive patients with suspected CAD for 5.7 years. A follow up of cardiac death, MI or coronary revascularization occurring more than 90 days after CTA, occurred in 3.9% of subjects. Compared to the NRS and SSS, the strongest association with incidence MACE was for low attenuation plaque volume (HR 1.12, p less than 0.0001) as measured using semi-automated technique.
CT Angiography Vs Functional Testing (Diagnosing Atherosclerosis Vs Ischemia): -
For a comprehensive risk assessment and prevention of cardiovascular events, there is a requirement of diagnosis of both coronary atherosclerosis and myocardial ischemia. Stress testing and invasive coronary angiography are tools which are used commonly for this purpose. However, none of the two are appropriate tests for diagnosing coronary atherosclerosis. A negative stress test does not exclude coronary atherosclerosis requiring medical therapy. Invasive coronary angiography gives precise information about the coronary arterial lumen but does not examine arterial wall. As such, a “normal” invasive coronary angiogram does not exclude coronary atherosclerosis.
The conceptual scheme of using non-invasive modalities for diagnostic decision making in patients with suspected CAD, who should undergo ICA is primarily aimed to avoid unnecessary risk of ICA & reduce the cost of healthcare.
The commonly performed non-invasive stress test that utilizes a combination of stress (delivered by exercise or a pharmacologic agent) and imaging protocols (using echocardiography or myocardial perfusion imaging) have many limitations. Prevalence of coronary artery disease, adequacy of stress achieved, quality of imaging data, as well as inter or intra observer variability are the variables which may influence the test results. Among stress test, stress echocardiography was more likely to overestimate and myocardial perfusion imaging was more likely to underestimate the burden of ischemia especially in presence of multi vessel disease.
While studying clinical impact of non-invasive imaging test on the use of ICA, National Cardiovascular Data Registry, has shown a low diagnostic yield of non-invasive tests to detect significant CAD in patients undergoing invasive coronary angiography (ICA). Out of 661,063 patients undergoing elective ICA, 64% had prior non-invasive testing (78% were SPECT-MPI, 20% other Stress testing & 2% had CCTA, prior to ICA). While 81% of patients showed abnormal non-invasive findings before ICA, only 45% of patients had obstructive CAD with 50% stenosis by ICA.
In PROMISE trial (Prospective Multicenter Imaging Study for Evaluation of Chest Pain), patients with stable chest pain and intermediate pretest probability for obstructive coronary artery disease (CAD) were randomly assigned to functional testing (exercise electrocardiography, nuclear stress, or stress echocardiography) or coronary computed tomography angiography (CCTA). The primary endpoint was death, myocardial infarction or unstable angina hospitalization over follow up of 26.1 month. In this study, it was found that prevalence of normal test results as well as incidence rate of events was lower in CCTA arm compared to functional test arm 33.4% Vs 78.0%, 0.9% Vs 2.1%, P0.001. Promise trial concluded that anatomic assessment by CCTA provided significantly better prognostic information than functional testing. Around 54% of event (74/137) occurred in patients with non-obstructive CAD (1 – 69% stenosis). Majority of the clinical event over 2 years follow up occurred in patients without obstructive coronary artery disease or myocardial ischemia, indicating a significant risk burden undetected by conventional measures of test positivity. Moreover, normal CCTA, in contrast to completely normal functional test is highly unlikely to be associated with MACE for at least 2 years. This determination of “warranty period” is an important additional benefit of CCTA. Demonstration of individual ischemia on stress testing has been the mainstay of cardiac diagnostic testing; but have limitation because of diminished diagnostic accuracy when it is compared with the gold standard of invasive coronary angiography. The rate of non-obstructive CAD was found to be high (59%) for patients with positive functional test before undergoing invasive coronary angiography. Coronary computed tomography angiography (CCTA) has emerged as a non-invasive diagnostic modality of choice that directly visualizes the coronary anatomy with a reportedly high diagnostic accuracy. An effective get keeping function is defined when after the test is performed, therapeutic management is promptly targeted by the noninvasive test finding.
In landmark ischemia trial, though was not designed primarily to compare prognostic benefit of anatomic approach by CCTA Vs Functional testing for ischemia, it was found that among 8518 participants, with at least moderate ischemia enrolled in trial, 3339 participants, failed screening by functional testing. Moreover, in this trial among stable patients who had evidence of moderate to severe ischemia, on stress testing an initial invasive strategy compared to conservative strategy was not associated with a reduction in the primary outcome of cardiovascular death, myocardial infarction or hospitalization for unstable angina over a median follow up of three years.
The pathophysiology of acute coronary events involves many poorly understood interactions between altered atherosclerotic plaque & a thrombosis – promoting milieu, which only in “perfect storm” scenario can combine to result in a clinically relevant ischemic event. Because of many variables involved, it remains difficult to predict a perfect storm. CCTA is a well validated strategy to diagnose the extent & severity of atherosclerotic coronary artery disease. There is a complex relationship between coronary anatomy, ischemia and CV outcome data (COURAGE Trial). Emerging evidences favouring total atherosclerotic burden rather than ischemia as an ultimate determinant of cardiovascular outcomes.
Reynolds et al 2020, in the follow up analysis of ischemia trial, reported that anatomy defined by extent and burden of CAD on CCTA, was more predictive of mortality and MI, compared to the severity of ischemia.
Mancini et al, in their post hoc analysis of courage trial, found that anatomic burden was a consistent predictor of death, MI and acute coronary syndrome, compared to ischemia burden.
The result of ischemia trial and other studies have revolutionised the concept of managing atherosclerotic disease. Diagnosis of atherosclerosis rather than ischemia is gaining more emphasis and atherosclerotic disease of any severity whether obstructive or non-obstructive calls for intensive risk factor control and preventive therapy irrespective of symptomatic status of patient.
CCTA undoubtedly is a procedure of choice in current scenario, for diagnosis of atherosclerotic coronary artery disease. However, CCTA alone cannot independently determine the hemodynamic significance of coronary stenosis, due to its low specificity for identifying coronary stenosis that induces ischemia (Ref ICR, Hydun Lee Interventional Cardiology Review 2016; 11(2), 105-9).
There is unpredictable relationship between stenosis severity & ischemia. Further decision to undergo invasive coronary angiography may be unnecessary in sizeable number of cases with CCTA showing significant stenosis. In recent years with ground breaking & innovative bioengineering principles, coupled with clinical evidences, it has become possible to complement the anatomical assessment provided by CTA with functional data that represent ischemia. The functional significance of coronary artery disease documented by Coronary computed tomography angiography can be obtained by one of the three methods i.e.
- CT perfusion (CTP) imaging
- Transluminal contrast attenuation gradient (TAG) &
- Fractional Flow Reserve (FFR)
The utility of CTP is limited due to requirement for pharmacological drug administration, additional radiation and contrast medium for stress imaging. Similarly, the trans luminal contrast attenuation gradient (TAG) assessment of functional severity of CAD is limited by the fact that TAG only assess a contrast attenuation cooperating in the delay of coronary flow across the stenotic lesion in a coronary vessel in the rest condition and the severity of TAG is likely to be associated with anatomical stenotic severity of CAD but may not relate well to the functional ischemia.
Fractional flow reserve (FFR) defined as ratio of maximum flow in a stenotic artery to maximum flow if the same artery were normal, is an invasive technique to determine lesion-specific ischemia to guide decision making for revascularization.
Use of FFR has established stenosis severity as an unreliable indicator of ischemia, with approximately half of high-grade stenosis manifesting no ischemia. On the other hand, a significant proportion of non-obstructive lesion cause ischemia by FFR, emphasizing the importance of factors other than stenosis as critical to lesion specific ischemia. Atherosclerotic plaque characteristics (APC’s) by CTA – including aggregate plaque volume % (% APV), positive remodeling (PR), low attenuation plaque (LAP) and spotty calcification (SC) are associated with future coronary syndrome, their relationship to lesion ischemia was evaluated by Park et al by performing CT (n = 252) with FFR for 407 coronary lesions. They found that % APV was associated with 10% increased risk of ischemia per 5
References
- Richard W Harper and Brian S Ko (2011). A new algorithm for the management of stable coronary artery disease incorporating CT coronary angiography and fractional flow reserve: how we can improve outcomes and reduce costs. MJA Vol 194, No. 4, 21 Feb.
- Takor B. Arrey-Mbi, Seth M. Klusewitz, Todd C (2017). Villines. Long term prognostic value of coronary computed tomography angiography. Curr Treat Options Cardio Med; 19: 90
- M J Budoff, D. Dowe, J G Jollies (2008) et al. Diagnostic performace of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicentre ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. Journal of the American College of Cardiology, vol 52, No. 21, 1724 – 1732,
- Cho I, Chang HJ, Sung JM, Pencina MJ, Lin FY, Dunning AM, Achenbach (2012) et al CONFIRM Investigators. Coronary computed tomographic angiography and risk of all-cause mortality and nonfatal myocardial infarction in subjects without chest pain syndrome from the CONFIRM Registry (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry). Circulation. 126:304–313.
- Rine Nakanishi, Mathew J Budoff. (2104,) A New Approach in Risk Stratification by Coronary CT Angiography. Hindawi Publishing Corporation Scientifica Vol Article ID 278039.
- J K Min, A Dunning, F Y Lin (2011) et al. Age, and sex-related differences in all causes mortality risk based on coronary computed tomography angiography findings: results from the international multicentre CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes an International Multicenter Registry) of 23,854 patients without known coronary artery disease. Journal of the American College of Cardiology, vol 58, No. 8, 849 – 860,
- Cheruvu C, Precious B, Naoum C, Blanke P, Ahmadi A, Soon J (2016) et al. long-term prognostic utility of coronary CT angiography in patients with no modifiable coronary artery disease risk factors: results from the 5-year follow-up of the CONFIRM International Multicenter Registry. J. Cardiovasc Compute Tomogr.; 10: 22 – 7.
- F Y Lin, L J Shaw, A M Dunning (2011) et al. Mortality risk in symptomatic patients with non-obstructive coronary artery disease: a prospective 2-center study of 2,583 patients undergoing 64-detector row coronary computed tomographic angiography. Journal of American College of Cardiology, vol 58, No. 5, 510 – 519,
- M S Bittencourt, E Hulten, and B. Ghaghara. (2014). Prognostic value of non-obstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circulation: Cardiovascular Imaging,
- Blanke P, Naoum C, Ahmadi A, Cheruvu C, Soon J, Arepalli C, (2016) et al. long-term prognostic utility of coronary CT angiography in stable patients with diabetes mellitus. JACC Cardiovasc Imaging.; 9: 1280 – 8.
- J K Min, D S Berman, A Dunning (2012) et al. All-cause mortality benefit of coronary revascularization vs medical therapy in patients without known coronary artery disease undergoing coronary computed tomographic angiography: results from CONFIRM (COronary CT Angiography EvaluatioN for Clinical Outcomes: An InteRnational Multicenter Registry), European Heart Journal, vol 33, No. 24, 3088 – 3097.
- C V Bourantas, H M Garcia – Garcia, V Farooq (2013) et al. Clinical and angiographic charcteristics of patients likely to have vulnerable plaques: analysis from the PROSPECT study. JACC Cardiovascular Imaging, Vol 6, pp 1263 – 1272,
- S. Motoyama, T Kondo, M Sarai (2007) et al. Multislice computed tomographic characteristics of coronary lesions in acute coronary syndromes. Journal of the American College of Cardiology, vol 50, No. 4, pp 319 – 326,
- S. Motoyama, M Sarai, H Harigaya (2009) et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. Journal of the American College of Cardiology, vol. 54, No. 1, pp 49 – 57,
- N Ahmadi, V Nabavi, F Hajsadeghi (2011) et al. Mortality incidence of patients with non-obstructive coronary artery disease diagnosed by computed tomography angiography. The American Journal of Cardiology, Vol 107, No.1, pp 10-16,
- Feuchtner G, Kerber J, Burghard P, Dichitl W, Friedrich G, Bonaros N, (2016) et al. The high-risk criteria low-attenuation plaque < 60 hu and the napkin-ring sign are the most powerful predictors of mace: a long-term follow up study. Eur Heart J Cardiovasc Imaging
- Nadjiri J, Hausleiter J, Jahnichen C, Will A, Hendrich E, Martinoff S, (2016) et al. Incremental prognostic value of quantitative plaque assessment in coronary CT angiography during 5 years of follow up. J Cardiovasc Comput Tomogr. 10: 97 – 104.


