Research Article | DOI: https://doi.org/10.58489/2837-3367/006
The Topographic Location of The Nasolacrimal Duct as An Anatomical Reference Point for Surgical Procedures in Maxillofacial Surgery
- ÓSCAR DE LEÓN * 1
1 San Ignacio University Hospital. Carrera 7 40-62 Otorhinolaryngology and maxillofacial surgery service, Colombia.
*Corresponding Author: ÓSCAR DE LEÓN
Citation: ÓSCAR DE LEÓN. (2023). The Topographic Location of The Nasolacrimal Duct as An Anatomical Reference Point for Surgical Procedures in Maxillofacial Surgery. Journal of ENT and Healthcare. 2(1). DOI: 10.58489/2837-3367/006
Copyright: © 2023 ÓSCAR DE LEÓN, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 23 March 2023 | Accepted: 29 March 2023 | Published: 03 April 2023
Keywords: orthognathic surgery; nasolacrimal duct; epiphora; Le Fort I osteotomy; computed tomography.
Abstract
Summary
The study aimed to measure the distance of the nasolacrimal duct to adjacent anatomical structures in a sample of 150 CT scans from the San Ignacio University Hospital in Bogotá, Colombia, in 2021. The data was collected in a retrospective observational study based on non-probabilistic sampling. The results showed that the length of the nasolacrimal duct is greater in men than in women and decreases as age increases. The study highlights the need for studies that consider the specific characteristics of the Latin American population to establish reference points for surgical procedures in maxillofacial surgery.
Introduction
In maxillofacial surgery, there are different surgical procedures that involve the craniofacial component and its bony, vascular, nervous, muscular, and glandular structures. Among these, the nasolacrimal duct is of great interest, as it is bordered medially by the palatine bone and the inferior turbinate in the nose and laterally by the maxillary bone, finally emptying into the inferior meatus [1]. Therefore, it is a structure that can easily be injured when performing maxillofacial, otorhinolaryngological, and ophthalmic surgical procedures [2,3,4]. Among the different forms of nasolacrimal duct injury reported in the literature, functional obstruction due to soft tissue edema can occur, which is secondary to maxillectomies, maxillary or nasal osteotomies, midface fractures, and antrostomies. This nasolacrimal obstruction that follows these events usually occurs early during the postoperative phase and is typically transient and self-limiting, creating a temporary functional blockage to tear passage [5,6]. Rarely does surgical interruption of the nasolacrimal system lead to permanent obstruction, but if it does, it results in persistent or recurrent epiphora, dacryocystitis, or hemolacria [7].
Young and Bell [2] establish an average measure of the location of the nasolacrimal duct, which is 11 to 17 mm from the piriform rim to the duct outlet, and they establish an average of 14 mm. Currently, this measure is maintained as a reference point to avoid injury to the nasolacrimal apparatus. However, published articles use the Anglo-Saxon or Asian phenotype as a reference and not the Latin American population, which could be a limiting factor in the average measurement of the nasolacrimal duct, resulting in injuries to the nasolacrimal component. In maxillofacial surgery, the literature associated with nasolacrimal apparatus injuries during surgical procedures is very limited. Currently, there are few reports, and most of them are in Anglo-Saxon populations, with phenotypic characteristics different from Latinas.
The objective of this study was to investigate, in a sample of computed tomography (CT) scans of the Kanteron system patients from the San Ignacio University Hospital, whether there is variation in anatomical measurements in different tomographic sections of the nasolacrimal duct and whether these influence or not when performing surgical interventions of the craniofacial skeleton.
Materials And Methods
Prior to the approval of the ethics committee of the San Ignacio University Hospital and the Faculty of Dentistry at Javeriana University, a non-interventional descriptive retrospective observational study was conducted. The population consisted of tomographies of patients treated in the Otorhinolaryngology and Maxillofacial Surgery service at the San Ignacio University Hospital (HUSI) in Bogotá - Colombia during 2021, whose face and paranasal sinuses tomography was taken at HUSI under the necessary parameters of position (parallel to the floor) and equipment characteristics in milliamperage and stipulated kilovoltage, where a volumetric helical acquisition is performed with a 64-line multi-detector CT scanner (coronal plane parallel to the ascending branch of the jaw). Subsequently, the CT scans were visualized and measured in the hospital system: Kanteron. Adult patients over 18 years of age, both healthy males and females from the intrahospital institutional system (KANTERON) were included. CT scans of patients with pre-existing systemic diseases or alterations that compromise the nasolacrimal duct, those who have had ablative surgical procedures in the nasomaxillary component, with a history of previous orthognathic surgery presenting material osteosynthesis in the upper jaw, or with any type of anomaly or tumor in the nasomaxillary zone, as well as those with a history of trauma in the middle third, were excluded, discarding their images as they were considered to affect the usual anatomy of the duct.
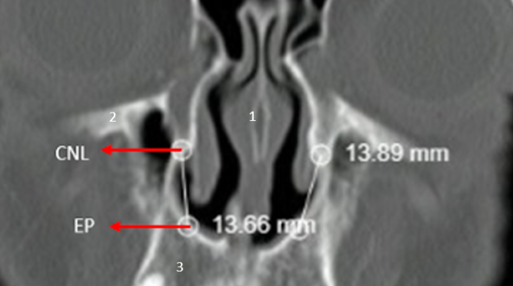
The measurement tool of the viewer was used to locate the specific anatomical points on the computer screen and adequately quantify the distances stipulated in the study. Magnification was used to minimize measurement error. The measurements taken were:
Coronal plane Measurement from piriform aperture (PA) to Nasolacrimal Duct (NLD)
- Septum
- Orbital floor
- Maxilla
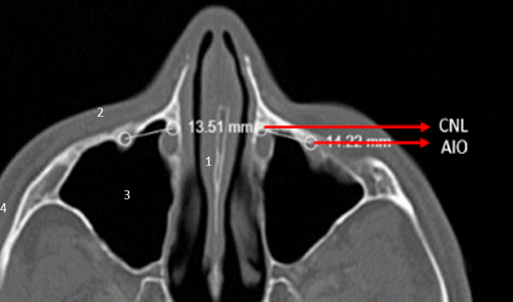
Axial plane Measurement from Infraorbital Foramen (IF) to Nasolacrimal Duct (NLD)
- Septum
- Anterior wall of maxillary sinus
- Maxillary sinus
- Zygomatic arch
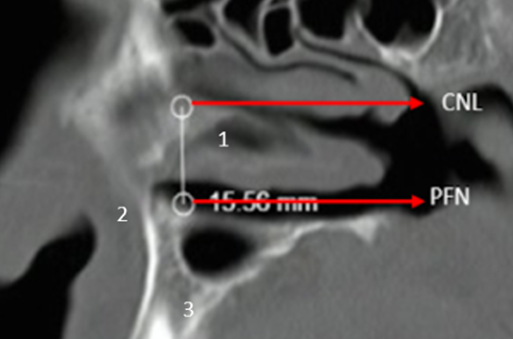
Sagittal plane Measurement from the floor of the nasal fossa (NF) to the Nasolacrimal Duct (NLD)
- Inferior turbinate
- Anterior nasal spine
- Maxilla
For the collection of data, a spreadsheet instrument was used in Excel, in which the variables sex, age, and measurement from piriform aperture to nasolacrimal duct, from infraorbital foramen to nasolacrimal duct, and from the floor of the nasal fossa to nasolacrimal duct in axial, sagittal, and coronal cuts (right and left sides) were recorded in millimeters. Images were added in the three tomographic cuts: axial, sagittal, and coronal with specific measurements in each tomography and each cut. A previous measurement was made for each cut and the corresponding anatomical reference until the measurement process was unified, and later applied to the topographies of the selected sample. The measurements were repeated three times for each CT and on the same coordinates, and subsequently, the instrument was completed by the two previously calibrated researchers. The information analysis was performed after the exploratory analysis, in which the quality of the entered records was controlled. Quantitative measurements were described based on summary measures such as mean and median, dispersion, standard deviation, and interquartile range. Qualitative measurements were described based on absolute and relative frequencies, and subsequently, the comparison by sex was made using U Mann Whitney hypothesis tests and t-tests for independent samples, according to the verification of normality and equality of variances assumptions (ratio of variances). The correlation with age was performed using Spearman's rho, and significant correlations were determined. All comparisons were made with α=0.05 to assess their significance and obtain results comparing them with previous studies and achieving extrapolated results to the surgical field in maxillofacial procedures.
Results
150 patient tomographies were included, with equal distribution regarding sex (50% men and 50% women). The average age of the patients was 43.15 years, 25% of the patients were up to 27.45 years old, 50% at most 35.73 years old, and 75% up to 61.97 years old.
The analysis of measurements according to age categories showed in general that there is a progressive decrease in the mean measurement of each of the cuts, in accordance with the progression of age by decade groups (see table 1).
Table 1. Mean measurements in each of the cuts (views) according to age decade groups.
CATEGORIZED AGE | CORONAL (PIRIFORM APERTURE-NASOLACRIMAL DUCT) RIGHT | CORONAL (PIRIFORM APERTURE-NASOLACRIMAL DUCT) LEFT | AXIAL (INFRAORBITAL FORAMEN-NASOLACRIMAL DUCT) RIGHT | AXIAL (INFRAORBITAL FORAMEN-NASOLACRIMAL DUCT) LEFT | SAGITTAL (FLOOR OF NASAL CAVITY- NASOLACRIMAL DUCT) RIGHT | SAGITTAL (FLOOR OF NASAL CAVITY- NASOLACRIMAL DUCT) LEFT |
Up to 30 years old | 14,42 | 14,39 | 14,88 | 14,84 | 15,65 | 15,60 |
From 30.01 to 40 years old | 14,12 | 14,16 | 14,43 | 14,56 | 15,69 | 15,67 |
From 40,01 to 50 years old | 14,30 | 14,38 | 14,57 | 14,64 | 14,88 | 14,93 |
From 50,01 to 60 years old | 14,27 | 14,41 | 14,72 | 14,81 | 14,95 | 14,70 |
From 60,01 to 70 years old | 13,90 | 13,94 | 14,14 | 14,00 | 15,81 | 15,80 |
From 70,01 to 80 years old | 13,67 | 13,67 | 13,94 | 13,95 | 15,14 | 15,19 |
over 80.01 years old | 13,41 | 13,49 | 13,70 | 13,77 | 16,18 | 16,09 |
In relation to the comparison of measurements by sex, it was observed that the age was similar in men and women, while significant differences (p<0>0.05). The measurements and statistical tests performed are shown in Table 2.
Table 2. Measurements of the nasolacrimal duct according to sex.
Variable | Gender | Media | D.E. | Itself. | F | p* | Dif media | Inf | U |
CORONAL (PIRIFORM APERTURE-NASOLACRIMAL DUCT) RIGHT | FEMALE | 13,85 | 1,12 | 0,130 | 0,169 | 0,005 | 0,59
| 0,19
| 1,00
|
MALE | 14,44 | 1,38 | 0,000 | ||||||
CORONAL (PIRIFORM APERTURE-NASOLACRIMAL DUCT) LEFT | FEMALE | 13,89 | 1,10 | 0,379 | 0,293 | 0,006 | 0,55
| 0,16
| 0,95
|
MALE | 14,44 | 1,32 | 0,001 | ||||||
AXIAL (INFRAORBITAL FORAMEN-NASOLACRIMAL DUCT) RIGHT | FEMALE | 14,33 | 1,69 | 0,494 | 0,771 | 0,233 | 0,34
| -0,22
| 0,89
|
MALE | 14,66 | 1,75 | 0,009 | ||||||
AXIAL (INFRAORBITAL FORAMEN-NASOLACRIMAL DUCT) LEFT | FEMALE | 14,38 | 1,70 | 0,420 | 0,666 | 0,355 | 0,26
| -0,30
| 0,83
|
MALE | 14,65 | 1,78 | 0,005 | ||||||
SAGITTAL (FLOOR OF NASAL CAVITY- NASOLACRIMAL DUCT) RIGHT | FEMALE | 15,22 | 1,69 | 0,107 | 0,915 | 0,045 | 0,57
| 0,01
| 1,14
|
MALE | 15,80 | 1,78 | 0,066 | ||||||
SAGITTAL (FLOOR OF NASAL CAVITY- NASOLACRIMAL DUCT) LEFT | FEMALE | 15,16 | 1,68 | 0,248 | 0,659 | 0,028 | 0,64 | 0,07 | 1,21 |
MALE | 15,80 | 1,85 | 0,110 |
T-test for independent means difference. α=0.05.
** U Mann Whitney test for median difference. α=0.05.
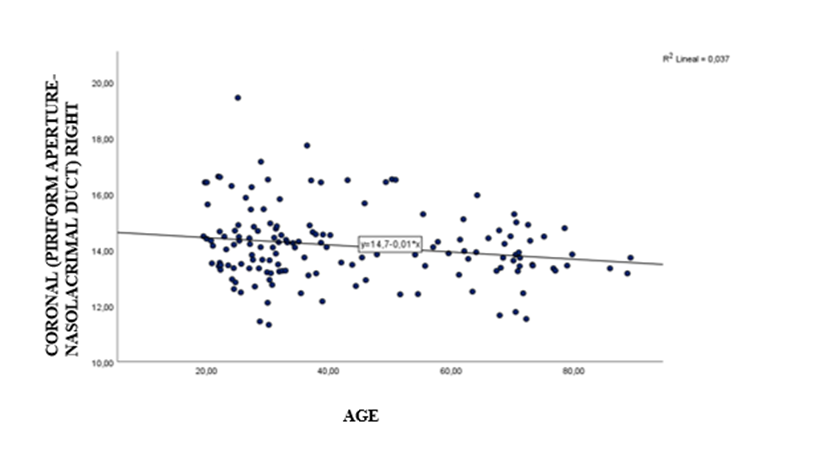
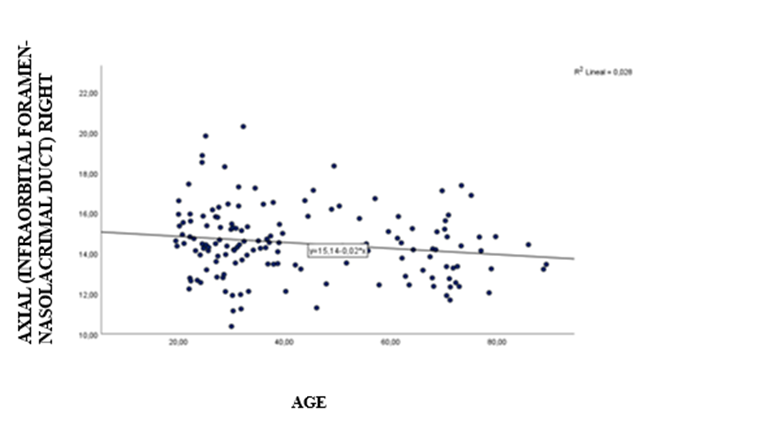
The correlation analysis of the measurements with age showed in general inverse correlations that indicate that as age increases, the magnitude of the measurement decreases (see figures 1 and 2); however, this correlation was significant only for the right coronal and right axial measurements; the correlation values are described in Table 3.
Table 3. Correlation of nasolacrimal duct measurements in different planes with age.
Variable | Rho de Spearman | p | IC 95% | |
CORONAL (PIRIFORM APERTURE-NASOLACRIMAL DUCT) RIGHT | -0,163 | 0,046* | -0,320 | 0,002 |
CORONAL (PIRIFORM APERTURE-NASOLACRIMAL DUCT) LEFT | -0,159 | 0,052 | -0,316 | 0,006 |
AXIAL (INFRAORBITAL FORAMEN-NASOLACRIMAL DUCT) RIGHT | -0,178 | 0,030* | -0,333 | -0,013 |
AXIAL (INFRAORBITAL FORAMEN-NASOLACRIMAL DUCT) LEFT | -0,159 | 0,051 | -0,316 | 0,006 |
SAGITTAL (FLOOR OF NASAL CAVITY- NASOLACRIMAL DUCT) RIGHT | -0,042 | 0,608 | -0,206 | 0,124 |
SAGITTAL (FLOOR OF NASAL CAVITY- NASOLACRIMAL DUCT) LEFT | -0,018 | 0,830 | -0,182 | 0,148 |
*Significant correlation at α=0.05 level.
Discussion
Surgical interventions in the nasomaxillary component are frequently performed by maxillofacial surgeons, otorhinolaryngologists, and ophthalmologists, where the nasolacrimal duct is a structure prone to injury. Therefore, measuring the opening of the duct with respect to adjacent anatomical structures that are easily identifiable becomes a useful method to establish a reliable and reproducible relationship and thus avoid injury to the nasolacrimal complex during surgical interventions.
Anatomically, the components of the lacrimal system are divided into secretory, distributive, and excretory systems, and two segments: distal and proximal. The proximal segment includes the canaliculi and lacrimal puncta, while the distal segment includes the lacrimal sac and nasolacrimal duct (NLD) [1, 2, 4]. The lower third of the lacrimal sac is particularly vulnerable to injuries due to the lack of fibrous protection. The nasolacrimal duct runs through the bony canal in a posterior-inferior direction and drains into the inferior meatus through the Hasner valve [3, 4]. It is bordered medially by the palatine bone and the inferior turbinate, laterally by the maxillary bone, and opens below the inferior meatus of the nose. Therefore, the lateral nasal wall is a complex anatomical and physiological structure [8]. The NLD is a continuation of the lacrimal sac, which has an intraosseous portion of approximately 12 mm and an intrameal portion of approximately 5 mm [4].
Obstructions of the NLD occur due to multifactorial mechanisms that can be divided into primary (or congenital) and secondary related to infectious, inflammatory, or mechanical etiologies that may be associated with surgical procedures such as turbinectomies, frontal sinus surgeries, maxillary osteotomies, external or endoscopic maxillectomies, rhinoplasties, reduction and fixation of facial fractures, among others [4,9]. These procedures can damage the NLD and produce ocular conditions such as posttraumatic epiphora or lead to obstruction of lacrimal flow due to edema in soft tissues resulting in the involvement of the nasolacrimal complex [10-14]. Small changes in the diameter of the bony nasolacrimal canal whose normal values have been evaluated by several studies can cause these types of conditions [15]. Shoshani et al. [16] reported on a patient who presented with epiphora and signs of dacryocystitis 2 weeks after orthognathic surgery. After the failure of conservative treatment, the patient required dacryocystorhinostomy (DCR). The possible etiological factors were the anatomical variation of the distance between the Hasner valve and the nasal floor and the tearing of the mucosa during lateral nasal wall osteotomy. Marais and Brookes [11] reported a case of secretory rhinopathy and hypersecretion of the lacrimal gland, which presented as a complication after Le Fort I surgery. Additionally, different secondary ophthalmological complications have been reported in cases of Le Fort I osteotomies in orthognathic surgery, where several cases of nasolacrimal duct obstruction have been presented: one reported by Shoshani et al. [16], one by Keller and Sather [17]. Cases of CNL obstruction were treated with dacryocystorhinostomy (DCR). When it comes to facial trauma, fractures in the mid-facial region can cause discontinuity in the bones affecting the maxilla, palate, zygomaticomaxillary complex, nasal bones, orbits, nasal-orbital-ethmoid complex, frontal sinus, and the lacrimal-nasal component. This can cause epiphora, diplopia, enophthalmos, hypoglobus, or depression of the malar region. Therefore, performing osteotomy and fixation with appropriate osteosynthesis material, making adequate reconstructions, and avoiding subsequent injuries to the nasolacrimal complex corrects the patient's symptoms [18].
For this reason, one simple way to prevent nasolacrimal apparatus injuries are additional, consistent, and identifiable anatomical landmarks that allow for easy and precise procedures in the maxillary region when the anatomy may not be straightforward, achieving satisfactory and predictable results.
Clinical examination of nasolacrimal function includes inspection of any visible lesion on the medial wall of the orbit, evaluation of nasolacrimal system permeability, and determination of the level of obstruction [7]. However, appropriate imaging examination of the lacrimal drainage system allows for the documentation of any obstruction, which is why tomographies are of great help in obtaining findings and, in the case of our study, quantifying their size to avoid injury [7]. Numerous studies [4,8,19] have used computed tomography as a tool to detail the anatomy of the nasolacrimal system and how variations in it can relate to drainage dysfunction. Most of these reports focus on structural variations such as CNL diameter, length in relation to anatomical references, nasolacrimal volume, or angle of the duct in relation to its outlet [20].
There are few studies that correlate anthropometric measurements between men and women with possible anatomical variations of the nasolacrimal duct (CNL). In this study, significant differences (p<0>
This study is not without limitations. The study is not different from others previously conducted regarding the emergence of the nasolacrimal duct in relation to anatomical structures, which remained stable in the axial, sagittal, and coronal sections with the selected anatomical reference points. However, it is important to note the greater accessibility that these points (nasal fossa, piriform aperture, and infraorbital nerve) have in providing a safe and easily measurable intraoperative margin in any surgical procedure that could injure the nasolacrimal duct. Additionally, the precision of the technique used is limited by the thickness of the tomographic slices, and for future studies, cuts of 1mm or less are recommended to avoid inaccuracies or difficulties in measuring CNL references. Finally, since this study focused on a population of healthy patients, these findings cannot be used to draw conclusions about the anatomy of patients with CNL pathology, but several important anatomical relationships were described that support bases that can be studied in the future.
Conclusions
The study results coincide with data published in previous studies regarding the measurement of the duct. In terms of sex distribution, the distance of the nasolacrimal duct is greater in men than in women, and in the age distribution, it showed generally inverse correlations indicating that as age increases, the magnitude of the measurement decreases.
Recommendations
This research project provides a basis for future studies that allow extrapolation of the results to the surgical environment. It is recommended to perform a similar study with a much larger sample to verify our results, as the limitation in our case was the number of included tomographies, as many did not meet the inclusion criteria. Additionally, the same measurements could be compared in different groups of people with Class I, II, and III dentofacial anomalies, and look for any type of variability in the position of the nasolacrimal duct and the possibility of finding significant differences that allow the clinician to make better decisions at the time of virtual planning of orthognathic or trauma surgery to avoid injuring the nasolacrimal duct or adjacent anatomical structures.
References
- Lin, Z., Kamath, N., & Malik, A. (2021). Morphometric differences in normal bony nasolacrimal anatomy: comparison between four ethnic groups. Surgical and Radiologic Anatomy, 43(2), 179-185.
View at Publisher | View at Google Scholar - You, Z. H., Bell, W. H., & Finn, R. A. Location of the nasolacrimal canal in relation to the high Le Fort I osteotomy. Journal of oral and maxillofacial surgery, 1992 50 (10), 1075-1080.
View at Publisher | View at Google Scholar - Brookes, C. D., Golden, B. A., Lawrence, S. D., & Turvey, T. A. Unilateral mydriasis after maxillary osteotomy: a case series and review of the literature. Journal of Oral and Maxillofacial Surgery, 2015 73(6), 1159-1168.
View at Publisher | View at Google Scholar - Ozcan, E. M., Dergin, G. Ü. H. A. N., & Basa, S. Prevalence of nasolacrimal canal obstruction and epiphora following maxillary orthognathic surgery. International journal of oral and maxillofacial surgery, 2018.47(6), 715-720.
View at Publisher | View at Google Scholar - Hueto-Madrid, J. A., & Gutierrez-Santamaria, J. (2012). Surgical complications of orthognathic surgery: presentation of three cases and review of the literature. Spanish Journal of Oral and Maxillofacial Surgery, 34(2), 56-74.
View at Publisher | View at Google Scholar - Loureiro, R. M., Collin, J., Sumi, D. V., Araújo, L. C., Murakoshi, R. W., Gomes, R. L. E., & Daniel, M. M. (2021). Postoperative CT Findings of Orthognathic Surgery and its Complications: A Guide for Radiologists. Journal of Neuroradiology.
View at Publisher | View at Google Scholar - Humber, C. C., Lanigan, D. T., & Hohn, F. I. (2011). Retrograde hemorrhage (hemolacria) from the lacrimal puncta after a Le Fort I osteotomy: a report of 2 cases and a review of the literature. Journal of Oral and Maxillofacial Surgery, 69(2), 520-527.
View at Publisher | View at Google Scholar - Okumuş, Ö. (2020). Investigation of the morphometric features of bony nasolacrimal canal: a cone-beam computed tomography study. Folia Morphologica, 79(3), 588-593.
View at Publisher | View at Google Scholar - GuptaN. An Overview of Nasolacrimal Duct (NLD) Encountered in Different Situations; Identification, Prevention and Management of NLD Injuries. Endoscopic Dacryocystorhinostomy, 2021 18 (6) 215-222.
View at Publisher | View at Google Scholar - Humber, C. C., Lanigan, D. T., & Hohn, F. I. (2011). Retrograde hemorrhage (hemolacria) from the lacrimal puncta after a Le Fort I osteotomy: a report of 2 cases and a review of the literature. Journal of Oral and Maxillofacial Surgery, 69(2), 520-527.
View at Publisher | View at Google Scholar - Marais J, Brookes GB. Secretomotor rhinopathy after Le Fort I maxillary osteotomy. Case report. Int J Oral Maxillofac Surg 1993; 22:17–9.
View at Publisher | View at Google Scholar - Tucker, N., Chow, D., Stockl, F., Codère, F., & Burnier, M. Clinically suspected primary acquired nasolacrimal duct obstruction: clinicopathologic review of 150 patients. Ophthalmology, 1997104 (11), 1882-1886.
View at Publisher | View at Google Scholar - Demas, P. N., & Sotereanos, G. C. (1989). Incidence of nasolacrimal injury and turbinectomy-- associated atrophic rhinitis with Le-Fort-I osteotomies. Journal of cranio-maxillofacial surgery: official publication of the European Association for Cranio – Maxillo - Facial Surgery, 1997 17(3), 116-118.
View at Publisher | View at Google Scholar - Ku, J. K., Yun, P. Y., Kim, Y. K., & Kim, J. H. Dacryolith after a Le Fort I fracture: case report. International journal of oral and maxillofacial surgery, 202049(9), 1199-1201.
View at Publisher | View at Google Scholar - Little, C., Mintz, S., & Ettinger, A. C. (1991). The distal lacrimal ductal system and traumatic epiphora. International journal of oral and maxillofacial surgery, 20(1), 31-35.
View at Publisher | View at Google Scholar - Shoshani, Y., Samet, N., Ardekian, L., & Taicher, S. (1994). Nasolacrimal duct injury after Le Fort I osteotomy. Journal of oral and maxillofacial surgery, 52(4), 406-407.
View at Publisher | View at Google Scholar - Keller, E. E., & Sather, A. H. (1990). Quadrangular Le Fort I osteotomy: Surgical technique and review of 54 patients. Journal of oral and maxillofacial surgery, 48(1), 2-11.
View at Publisher | View at Google Scholar - Brookes, C. D., Golden, B. A., Lawrence, S. D., & Turvey, T. A. (2015). Unilateralmydriasis after maxillary osteotomy: a case series and review of the literature. Journal of Oral and Maxillofacial Surgery, 73(6), 1159-1168
View at Publisher | View at Google Scholar - McCormick A, Sloan B. The diameter of the nasolacrimal canal measured by computed tomography: gender and racial differences. Clin Exp Ophthalmol. 2009; 37(4): 357–361.
View at Publisher | View at Google Scholar - Ipek E, Esin K, Amac K, et al. Morphological and morphometric evaluation of lacrimalgroove. Anat Sci Int 2007; 82:207–10.
View at Publisher | View at Google Scholar - Maskey, S., & Shrestha, R. (2019). Cephalometric approach to vertical facial height. Orthodontic Journal of Nepal, 9(1), 54-58
View at Publisher | View at Google Scholar - Ramey, N. A., Hoang, J. K., & Richard, M. J. (2013). Multidetector CT of nasolacrimal canal morphology: normal variation by age, gender, and race. Ophthalmic Plastic & Reconstructive Surgery, 29(6), 475-480.
View at Publisher | View at Google Scholar - Mendelson, B., & Wong, C. H. (2020). Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic plastic surgery,44(4), 1151-1158.
View at Publisher | View at Google Scholar - Shaw RB Jr, Kahn DM (2007) Aging of the midface bony elements: a three-dimensional computed tomographic study. Plast Reconstr Surg 119:675–68
View at Publisher | View at Google Scholar - Kahn DM, Shaw RB Jr (2008) Aging of the bony orbit: a threedimensional computed tomographic study. Aesthet Surg J 28:258–264
View at Publisher | View at Google Scholar - Levine RA (2008) Aging of the midface bony elements. PlastReconstr Surg 121:698–699
View at Publisher | View at Google Scholar - Pessa JE, Zadoo VP, Mutimer KL, Haffner C, Yuan C, DeWitt AI, Garza JR (1998). Relative maxillary retrusion as a natural consequence of aging: combining skeletal and soft tissue changes into an integrated model of midfacial aging. Plast Reconstr Surg102:205–212
View at Publisher | View at Google Scholar