Case Report | DOI: https://doi.org/10.58489/2836-5828/007
Leukemia Infiltration Secondary Acute Renal Damage
1MD, Resident, Department of Internal Medicine, Ankara City Hospital, Ankara, Turkey,
2MD, Physician, Division of Nephrology, Ankara City Hospital, Ankara, Turkey.
3MD, Physician, Department of Pathology, Ankara City Hospital, Turkey.
4MD, Associate Professor, Department of Nephrology, Ankara City Hospital, Ankara, Turkey.
5MD, Professor, Department of Nephrology, Ankara City Hospital, Ankara, Turkey.
*Corresponding Author: Amed Trak, MD,
Citation: Amed Trak, (2023). Leukemia Infiltration Secondary Acute Renal Damage. Archives of Urology and Nephrology. 2(1). DOI: 10.58489/2836-5828/007
Copyright: © 2023 Amed Trak, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 27 February 2023 | Accepted: 24 March 2023 | Published: 03 April 2023
Keywords: Chronic lymphocytic leukemia,leukemic infiltration, acute renal damage.
Abstract
Chronic lymphocytic leukemia is a disease that it is developed by cumulation of mature-looking small lymphocytes in blood,bone marrow,lymph nodes,spleen and other lymphatic organs and tissues.It can be attained as asymptomatic lymphocytosis in old patients;on the other hand, kidney dysfunction can also be seen as a preliminary finding. Leukemia infiltration secondary acute renal damage can rarely be seen while renal damage is being occured because of many different reasons in chronic lymphocytic leukemia patients.Here,we aimed to review the literature by presenting 70-year-old patient who was under hematology follow-up due to chronic lymphocytic leukemia,who was hospitalized in our clinic because of acute kidney damage in routine examinations and was found to have leukemic infiltration in pathology.
Introduction
Chronic lymphocytic leukemia(CLL) is a disease that it is developed by the cumulation of mature-looking small lymphocytes in the blood, bone marrow, lymph nodes, spleen, and other lymphatic organs and tissues [1].It is known that chronic lymphocytic leukemia(CLL) can be accompanied by renal failure. Kidney failure incidence was found to %7,5 in a cohort study which was conducted by Mayo Clinic with more than 2000 CLL patients. [2] CLL’s renal damage reasons can be listed as ureteral obstruction caused by lymphadenopathy pressure, tumor lysis syndrome(TLS) which can be developed after treatment and direct kidney infiltration which is rarely being seen. Pathologies like light chain nephropathy, renal amyloidosis, membranoproliferative glomerulonephritis(MPGN), granulomatous interstitial nephrite, and minimal change disease were reported among other uncommon reasons.[2] Here; in a patient with CLL, our aim was to present a case with lymphoid cell infiltration in a kidney biopsy performed due to Acute Kidney Injury (AKI).
Case Presentation
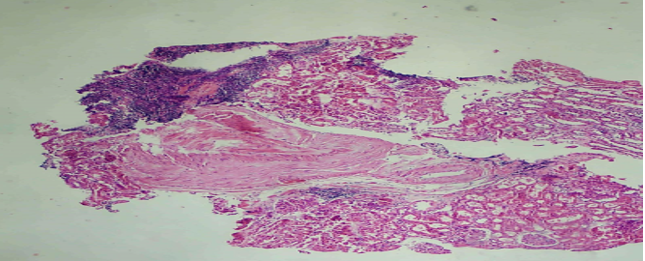
A 70-year-old male patient with a diagnosis of hypertension (HT), dementia, chronic obstructive lung disease, and stage 1 CLL for 1 year, with a creatinine of 1.1 mg / dL a month earlier and a creatinine value of 1.76 mg / dL in routine control, was hospitalized to our service with the diagnosis of AKI. It was learned that he was followed up in the Hematology Clinic due to stage 1 CLL and he was under conservative follow-up because immunosuppressive therapy was not seen as a necessity. The patient having had no active complaint in examination for AKI etiology did not have nephrotoxic agent usage history; besides, prerenal and postrenal reasons were also excluded. In the physical examination, blood pressure arterial was 140/90 mmHg, and cardiovascular, respiratory system and abdominal examination were normal. A diameter of 1.5 cm in the right axillary area and a diameter of 2 cm palpable lymphadenopathy in the right anterocervical area were pathologically identified. In the patient's laboratory values; urea: 52 mg / dL (<49>
Discussion
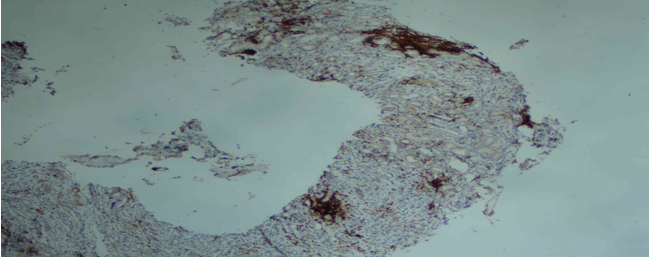
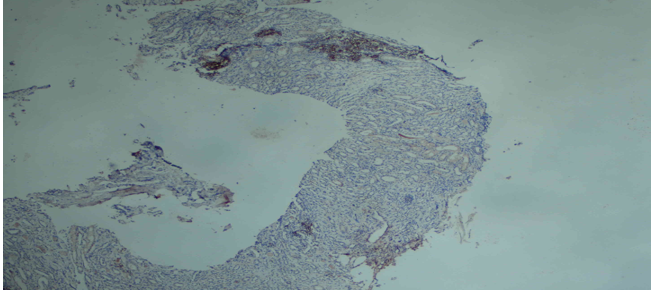
Chronic lymphocytic leukemia is a lymphoid malignancy characterized by the cumulation and increase of the mature CD5 + B cells in blood, bone marrow, and lymphoid tissues. [1] The average age in CLL is 71. The incidence frequency of the disease in the USA is 4.5/100.000. Male and female incidence rate is 2:1.The incidence get closer to each other as people grow older. They are seen at an equal rate in both sexes even at the ages over 80. [3] CLL diagnosis is made by the presence of over 5.000/μL mature B lymphocytes in peripheral blood at least for 3 months. .[4] For CLL; CD5, CD19, and CD23 are found in characteristic iimmunophenotypeswhereas CD20, surface immunoglobulin, CD79b, and FMC7 are barely found. .[4] If lymphocytes are positive with CD5, two possibilities are extremely high: CLL or mantle cell lymphoma(MCL).CD23 is generally positive in CLL cells; besides,it is possible to diagnose correctly because CD23 is negative in MCL.CLL renal involvement has been confirmed in our case by observing diffuse CD5, CD20, and CD23 staining in lymphoid cells.
In CLL which shows a highly variable clinical course; after the diagnosis, some of the patients are extremely silent and asymptomatic and live for many years without progressing, while some of them tend to progress rapidly although they are either advanced or early phase at the time of diagnosis. [5] In the patients who bhave started to the treatment; the most common signs and symptoms are fever,night sweating,weight loss,organomegaly, anemia associated with bone marrow failure and thrombocytopenia.[2]In CLL; AKI associated with infiltration is a very rarely seen complication despite the fact that it is reported at `-90 in renal involvement autopsy series. AKI can be detected as a first sign of CLL in some cases.It is presumed that leukemic infiltration causes a tubular obstruction even though kidney damage mechanism is not exactly known.[6] Except that,CLL also causes gromerular pathologies.MPGN (6) and membranous nephropathy () are the mostly encountered gromerular pathologies [2]. The other rarely seen glomerulonephritis types are minimal change disease and focal segmental glomerulosclerosis.Tumor lysis syndrome in CLL is scarcely seen but it is thought that venetoclax, which is a bcl-2 inhibitor and used in the treatments of %6 of the patients, causes it. [2]
Another complication of CLL is amyloidosis. 18 (U) of the patients are diagnosed with AL amyloidosis with renal biopsy in a study including 33 CLL patients who are taking place in the literature. While plasma
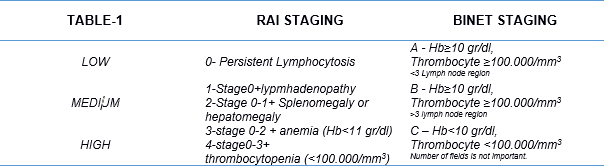
cell clones brought about amyloidosis in 14 of these patients,it was identfied that CLL clones caused amyloidosis in the other 4 patients. [7] Clinical staging system was based on defining prognosis in CLL;furthermore,only physical examination and peripheral smear are needed in determining clinical staging. [10] In the notifications published between 1966 and 1973, Rai et al. developed a CLL staging system that could prospectively differentiate patients based on their overall appearance for survival. [2] After that, a new classification was introduced by Binet et al. There have been some deficiencies although there is a meaningful relationship between stage and survival in both classifications. Modified Rai and Binet classification is stated in Table 1.[5] Patients with intermediate (Stage I and II) and high risk (Stage III and IV) according to the modified Rai classification or stages B and C according to the Binet classification generally benefit from treatment. Some of these patients (Rai intermediate risk and Binet stage B ) can be followed without treatment unless any progression symptoms or signs appear.[5]
AKI associated with leukemic infiltration was described in previously reported cases in the literature. Renal involvement couldn’t have been related to the staging in CLL patients. Renal involvement was shown by doing a biopsy and different chemotherapy regimens were applied to the cases involved in the literature. Kidney function recovery was observed as a result of the treatment and recovery of kidney functions via regression was also observed in some cases. [2]
As a result; leukemic infiltration should always be kept in mind when CLL patients apply with kidney dysfunction. The case we have presented is stage 1 CLL and there is no treatment indication in terms of hematology according to the current modified Rai and Binet classifications. It has been observed that renal functions also recover as a consequence of the treatment of primary disease with chemotherapy in AKI caused by renal infiltration in the literature. On the other hand; chemotherapy couldn’t have been given because of his being stage 1 in our case. It was observed that his creatinine value stopped at 1.5 mg/dL by the end of the 6th month of our polyclinical follow-ups. On account of this; we are agreed that along with liver and spleen involvement in the staging of CLL, lymphocytic infiltration proven by renal biopsy to be performed in the presence of accompanying renal dysfunction should be included in the classification, and CLL staging and chemotherapy indication should be re-evaluated, and cases accompanied by AKI should be given a chance to treat.
References
- Delgado, J., Nadeu, F., Colomer, D., & Campo, E. (2020). Chronic lymphocytic leukemia: From molecular pathogenesis to novel therapeutic strategies. Haematologica, 105(9), 2205.
View at Publisher | View at Google Scholar - Wanchoo R , Ramirez C.B., Barrientos J , Jhaveri K. et al “Renal Involvement in Chronic Lymphocytic Leukemia” Clin Kidney J 2018 Oct;11(5):670-680.
View at Publisher | View at Google Scholar - Jennifer A. Woyach, John C. Byrd Harrison, E. Braunwald, A. S. Fauci, D. L. Kasper et al, “Principles of Internal Medicine “ 1024–1034, McGraw-Hill, North America, 2018.
View at Publisher | View at Google Scholar - Hallek, M., Cheson, B. D., Catovsky, D., Caligaris-Cappio, F., Dighiero, G., Döhner, H., ... & Kipps, T. J. (2008). Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute–Working Group 1996 guidelines. Blood, The Journal of the American Society of Hematology, 111(12), 5446-5456.
View at Publisher | View at Google Scholar - Türkiye Hematoloji Derneği Ulusal Tedavi ve Tanı Klavuzu 2012 syf:3,6
View at Publisher | View at Google Scholar - Ferreira A.C, Brum S. Carvalho D., Pataca I, Carvalho F., Santos M.C., Santos J.R.,1 et al. “Renal dysfunction due to leukemic infiltration of kidneys in a case of chronic lymphocytic leukemia” Hemodialysis International 2010; 14:87–90
View at Publisher | View at Google Scholar - Kourelis, T. V., Gertz, M., Zent, C., Lacy, M., Kyle, R., Kapoor, P., ... & Dispenzieri, A. (2013). Systemic amyloidosis associated with chronic lymphocytic leukemia/small lymphocytic lymphoma. American journal of hematology, 88(5), 375-378.
View at Publisher | View at Google Scholar - Demir V, Kahraman S, Katgı A, et al. Kronik Lenfositik Lösemili Hastaların Genel Klinik Özelliklerinin Değerlendirilmesi. 9 Eylül Tıp Dergisi 2012;26:9-19.
View at Publisher | View at Google Scholar - Hewamana, S., Pepper, C., Jenkins, C., & Rowntree, C. (2009). Acute renal failure as the presenting feature of leukaemic infiltration in chronic lymphocytic leukaemia. Clinical and experimental nephrology, 13, 179-181.
View at Publisher | View at Google Scholar - Çağlıyan, G. A., Aslankarasoy, N., & Bilgir, O. Kronik Lenfositik Lösemili Hastaların Değerlendirilmesi: Tek Merkez Deneyimi 1.
View at Publisher | View at Google Scholar