Research Article | DOI: https://doi.org/10.58489/2836-5828/005
Impact of Appropriate Antibiotics within One Hour and Patients' Outcome: A Study and Review
- Srirupa Biswas 1*
- Sankha Dasgupta 1
- Moumita Majumder Bhowmick 1
- Smriti Gupta 1
- Dr.Saswati Sinha 1
- Dr. Sounak Ghosh 1
- Dr. Subhash Todi 1
- Dr.Pinaki Dutta 1
- Dr. Ketousetuo Kuotsu 1
1 AMRI Hospital, Dhakuria and Jadavpur University, West Bengal.
*Corresponding Author: Srirupa Biswas
Citation: Srirupa Biswas, Sankha Dasgupta, Moumita Majumder Bhowmick, Smriti Gupta, et.al (2023), Impact of Appropriate Antibiotics within One Hour and Patients' Outcome: A Study and Review, Archives of Urology and Nephrology.1(1). DOI: 10.58489/2836-5828/005
Copyright: © 2023 Srirupa Biswas, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Received: 18 February 2023 | Accepted: 24 February 2023 | Published: 28 February 2023
Keywords: antibiotics; patients' outcome; review
Abstract
Background: Rapid initiation of antibiotic treatment is considered crucial in patients with severe infections such as septic shock & bacterial meningitis. The initiation of treatment with inappropriate antimicrobial agents (in relation to the subsequently demonstrated sensitivity of the pathogen) as the initial empiric therapy may be the single most common cause of prolonged delays in the introduction of effective therapy. Only in 5% of cases were antibiotics administered within 1 hr of the decision making, in 47% of cases it took 1–2 hrs. Only in 33% of cases antibiotics were prescribed within one hour of decision making. In 95% of cases antibiotics were administered within one hour of prescription. Sepsis is the main cause of death in patients treated in intensive care units (ICU). Current sepsis guidelines recommend administration of antibiotics within one hour of ED triage. However, the quality of supporting evidence is moderate & studied have shown mixed results regarding the association between antibiotics administration timing & outcome in septic shock.
Objective:The aim of this study was to assess whether timing of administration of appropriate antibiotics within one hour of admission to the ICU impact patient outcomes.
Method: Timing of ICU admission noted from the patient’s ICU nursing chart when the first vital parameters are noted by the nurse. Timing of administration of 1st dose of antibiotic and antibiotic that is administered within the first one hour of admission is noted from ICU nursing chart (in minutes from the timing of ICU admission). Appropriateness of antibiotic is assessed from the microbiology culture and sensitivity result. Outcome measures is noted from the ICU database. Data is then recorded systemically in the data collection form and finally entered in the excel sheet for analysis. All the data is then analysed by statistician by appropriate statistical tests.
Result: A total of 53 patients, including 63.2% in the sepsis group and 53.4% in the septic shock group received antibiotics within the first hour. 87.5 % patients who received antibiotic within one hour of admission were discharged compared to 81.0% patients who received first dose of antibiotic beyond one hour of admission. The commonest gram-negative organisms were E. coli and Klebsiella in both groups. The commonest antibiotic administered was Meropenem in both groups. All patients who received appropriate antibiotic were discharged compared with only 69.2% patients discharged whose antibiotic choice was inappropriate. Mortality was 30.8% in the group whose initial antibiotic choice was inappropriate while no patients died in the group where the patient received appropriate empirical therapy.
Conclusion: In my study it is demonstrated that gram-negative bacteria remain the major pathogen in sepsis as has been demonstrated in most ICUs in India. When appropriateness as well as timing of administration were compared simultaneously, all patients who received appropriate antibiotic within one hour or more than one hour survived to discharge. However, if antibiotic choice was inappropriate, 25% patients died even if they received the antibiotics within one hour and if the first dose was delayed beyond the first hour, the mortality further increased to 40%. There was no significant difference in the mean of ICU length of stay and mean hospital length of stay of patients based on appropriateness of empirical antibiotic therapy.
Introduction
Rapid initiation of antibiotic treatment is considered crucial in patients with severe infections such as septic shock and bacterial meningitis, but may not be as important for other infectious syndromes. A better understanding of which patients can tolerate a delay in start of therapy is important for antibiotic stewardship purposes. Infections with a high bacterial burden, such as those seen in infective endocarditis, require treatment with antibiotics with rapid bactericidal activity. In most cases, more than 1 antibiotic is used to provide synergistic activity and rapid killing. Another factor that can affect the efficacy of antibiotics is their ability to penetrate and remain (for an adequate time) at the site of infection. The ability of antibiotics to penetrate necrotic tissues, abscesses, or biofilms also can limit their efficacy. Infections can be difficult to treat and require prolonged antibiotic courses [1].
Injudicious prescribing of antibiotics in the management of infectious diseases results in overprescribing of antibiotics and, ultimately, development of microbial resistance to antibiotics [2-4].In situations where antibiotics are selected presumptively, as occurs particularly in the empiric treatment of infections, inappropriate prescribing of antibiotics can pose a major problem in antibiotic usage. Prescribers in such instances may over-prescribe antibiotics in combinations to cover for diagnostic imprecision [5]. This is particularly common in developing countries where empiric prescribing of antibiotics is a mainstay of treating infections. Most developing countries lack functional or efficient systems of operating microbiology laboratories, a situation not conducive to routine identification and antibiotic sensitivity testing of pathogens [6,7].
Inappropriate prescribing of antibacterial agents is accepted as a cause of treatment failures and increased costs of treating infections [8]. Inappropriate prescribing has been associated with microbial resistance development to antibiotics, and successful intervention studies to improve antibiotic prescribing have actually been found to reduce antimicrobial resistance [9]. Timely antibacterial treatment is associated with reduced length of hospital stays and reduced mortality [10,11]. Therapeutic deficiencies identified with some antibiotic prescriptions may not be seen as results of inappropriate prescribing, particularly in settings where the drugs are prescribed in combination to treat infections empirically. It is possible for only a subset of such prescribed antibiotics to be effective against the pathogens causing the infection, making the therapeutic infectiveness of others in the prescribed set less obvious. In other circumstances, as seen for example in cases of viral infections closely mimicking bacterial infections in clinical presentations, patients’ recovery may not in any way be attributable to prescribed antibiotics [12]. Prescribers may interpret outcomes of treatments they offered in all these instances as results of the effectiveness of the prescribed antibiotics, potentially eliminating their recognition of therapeutic inadequacies of ill prescribed antibiotics. Together, these situations explain the perpetuation of inappropriate prescribing of antibiotics in clinical practice despite the negative effects the practice has on patient management for infections. Studies that investigate the impacts of appropriately and inappropriately prescribed antibiotics on treatment outcome parameters are scarce. We believe that prescribers may become less resistant to prescribing antibiotics appropriately if they are aware of the impacts antibiotic prescribing have on treatment outcomes [13].
Review Of Literature:
1. In 2018, Richard Y Kim et al, did a study on Antibiotic Timing and Outcome in Sepsis. An observational cohort study was conducted on 117 patients who came through the University of Louisville Hospital ED and subsequently were directly admitted to the intensive care unit (ICU). They found no significant association between time in the ED (emergency department) and mortality between survivors and non-survivors (5.5 versus 5.7 hours, P = 0.804). After adjusting for expected mortality, a 22% increase in mortality risk was found for each hour delay from triage to antibiotic(s) ordered; a 15% increase in mortality risk was observed for each hour from triage to antibiotic(s) given. Both time from triage to antibiotic(s) ordered (hazard ratio [HR] = 0.8, P = 0.044) and time from triage to antibiotic(s) delivery (HR = 0.79, P = 0.0092) were independently associated with an increased hospital stay (HR = 0.79, P = 0.0092). They concluded that though no significant association between mortality and ED time was demonstrated, we observed a significant increase in mortality in septic patients with both delays in antibiotic(s) order and administration. Delay in care also resulted in increased hospital stays both overall and in the ICU.
2. In 2017, Robert Sherwin et al, conducted a study on Does Early and Appropriate Antibiotic Administration Improve Mortality in Emergency Department Patients With Severe Sepsis or Septic Shock? It included studies were randomized controlled trials, meta-analyses, prospective trials, and retrospective cohort studies. These studies were identified by a rigorous search methodology. No review articles, case series, or case reports were included. Predefined criteria were used to evaluate the quality and appropriateness of selected articles as part of a structured review. It concluded that patients with severe sepsis and septic shock should receive early and appropriate antibiotics in the emergency department. Patients with septic shock who received appropriate antimicrobial therapy within 1 h of recognition had the greatest benefit in mortality.
3. In 2017, Vincent X Liu et al, studied The Timing of Early Antibiotics and Hospital Mortality in sepsis. It was a retrospective study of 35,000 randomly selected inpatients with sepsis treated at 21 emergency departments between 2010 and 2013 in Northern California. The primary exposure was antibiotics given within 6 hours of emergency department registration. The primary outcome was adjusted in-hospital mortality. They used detailed physiologic data to quantify severity of illness within 1 hour of registration and logistic regression to estimate the odds of hospital mortality based on antibiotic timing and patient factors. They concluded that in a large, contemporary, and multicenter sample of patients with sepsis in the emergency department, hourly delays in antibiotic administration were associated with increased odds of hospital mortality even among patients who received antibiotics within 6 hours. The odds increased within each sepsis severity strata, and the increased odds of mortality were greatest in septic shock.
4. In 2015, Sarah A .Sterling et al, did a review and meta-analysis on The Impact of Timing of Antibiotics on Outcomes in Severe Sepsis and Septic Shock. It was performed using a pre-defined, written protocol of The Cochrane Database, CINAHL, PubMed, and Scopus databases with no start date to January 2015. The effect of time to antibiotic administration on mortality was assessed in two ways based upon the SSC (Surviving Sepsis Campaign) Guideline recommendations: a. Antibiotic administration within three hours of hospital presentation/ED triage; b. Antibiotic administration within one hour of severe sepsis/septic shock recognition. A total of 10,208 patients receiving antibiotics within 3 hours of triage of whom 2574 died and 5970 patients receiving antibiotics in 3 or more hours after triage of whom 1793 died. It was concluded that in patients with severe sepsis and septic shock, administration of antibiotics within three hours of ED triage or within one hour of recognition of severe sepsis/septic shock did not confer mortality benefit. These results suggest that currently recommended specific timing metrics in international guidelines are not supported by the currently available evidence.
5. In 2014, Ferrer, Ricard et al, conducted a study on Empiric Antibiotic Treatment Reduces Mortality in Severe Sepsis and Septic Shock from the First Hour. It was a retrospective analysis of a large database collected prospectively for the Surviving Sepsis Campaign. A total of 28,150 patients with severe sepsis and sepsis shock, from January 2005 through February 2010, were evaluated. The result of the analysis of this large population of patients with severe sepsis and sepsis shock demonstrate that delay in first antibiotic administration was associated with increased in-hospital mortality. In addition, there was a linear increase in the risk of mortality for each hour delay in antibiotic administration. These results underscore the importance of early identification and treatment of sepsis patients in the hospital setting.
6. In 2011, Michael A Puskarich et al, studied Association Between Timing of Antibiotic Administration and Mortality from Septic Shock in Patients Treated with a Quantitative Resuscitation Protocol. It was a preplanned analysis of a multicenter randomized controlled trial of early sepsis resuscitation. Of 291 included patients, mortality did not change with hourly delays in antibiotic administration up to 6 hours after triage. Mortality was significantly increased in patients who received initial antibiotics after shock recognition compared with before shock recognition; however, among patients who received antibiotics after shock recognition, mortality did not change with hourly delays in antibiotic administration. It was concluded that in the large, prospective study of emergency department patients with septic shock, found no increase in mortality with each hour delay to administration of antibiotics after triage. However, delay in antibiotics until after shock recognition was associated with increased mortality.
7. In 2010, ShahlaSiddiqui and JunaidRazzak, reviewed a study on Early versus late pre‐intensive care unit admission broad spectrum antibiotics for severe sepsis in adults to assess the difference in outcomes with early compared to late administration of antibiotics in patients with severe sepsis in the pre‐intensive care unit (ICU) admission period. They defined early as within one hour of presentation to the ED and planned to include randomized controlled trials of early versus late broad-spectrum antibiotics in adult patients with severe sepsis in the ED, prior to admission to the intensive care unit. It was concluded that they were unable to make a recommendation on the early or late use of broad-spectrum antibiotics in adult patients with severe sepsis in the ED pre‐ICU admission. There is a need to do large prospective double blinded randomized controlled trials on the efficacy of early (within one hour) versus late broad spectrum antibiotics in adult severe sepsis patients. Since it makes sense to start antibiotics as soon as possible in this group of seriously ill patients, administering such antibiotics earlier as opposed to later is based on anecdotal suboptimal evidence.
8. In 2010, Gaieski, David et al, conducted a study on Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. It was a single-center cohort study. The emergency department of an academic tertiary care center from 2005 through 2006. Two hundred and sixty-one patients undergoing early-goal therapy. This study suggested that elapsed time from triage and qualification of early goal-directed therapy to administration of appropriate antimicrobials are primary determinants of reduce mortality in patients with severe sepsis and septic shock treated with early goal- directed therapy.
9. In 2007, D. Lepur and B. Barsic, conducted a study on Community-Acquired Bacterial Meningitis in Adults: Antibiotic Timing in Disease Course and Outcome. Two hundred and eighty-six patients with community-acquired bacterial meningitis aged 14 years and more were included in this retrospective cohort study. Observational period was between 1 January 1990 and 31 December 2004. This study emphasizes the importance of early and adequate antibiotic treatment in the management of bacterial meningitis which significantly enhances the chances for favorable outcome.
10. In 2006, Kumar et al, studied the classic retrospective cohort study of 2,731 septic shock ICU patients. It showed a strong correlation between delay in effective antibiotic therapy and in-hospital mortality after recurrent or persistent arterial hypotension (P <0>in vitro activity for the isolated pathogenic microorganism or the underlying clinical syndrome).
11. In 2005, N. Proulx et al, did a retrospective study on Delays in the administration of antibiotics are associated with mortality from adult acute bacterial meningitis. They reviewed 123 cases of adult acute bacterial meningitis in 119 patients aged ≥16 years admitted to hospital from January 1990 to March 2002, using multivariate regression analysis to assess the association between meningitis mortality and door-to-antibiotic time. The study suggests that there is an independent incremental association between delays in administrating antibiotics and mortality from adult acute bacterial meningitis.
12. In 2004, Peter M. Houck et al, performed a retrospective study on Timing of Antibiotic Administration and Outcomes for Medicare Patients Hospitalized with Community-Acquired Pneumonia. They used medical records from a national random sample of 18209 Medicare patients older than 65 years who were hospitalized with community-acquired pneumonia from July 1998 through March 1999. Outcomes were severity adjusted mortality, readmission within 30 days of discharge, and length of stay (LOS). The concluded that antibiotic administration within 4 hours of arrival was associated with decreased mortality and LOS among a random sample of older inpatients with community-acquired pneumonia who had not received antibiotics as outpatients. Administration within 4 hours can prevent deaths in the Medicare population, offers cost savings for hospitals, and is feasible for most inpatients.
Aims and objective:
- To assess whether timing of administration of antibiotics within one hour of admission to the ICU impact patient outcomes.
- To assess whether appropriateness of the empiric antibiotic administered impact patient outcomes.
- Outcomes that will be assessed include:
- Primary outcome: ICU mortality
- Secondary outcomes:
- Hospital mortality
- ICU length of stay
- Hospital length of stay
- Need for mechanical ventilation
- Need for vasopressor support
- Need for dialysis
Study rationale:
Currently, there are no studies from India that have investigated the appropriateness of empiric therapy of antibiotics within one hour of admission to ICU impacts patients' outcome. Given the high prevalence of sepsis or septic shock patients in Indian ICUs, their high mortality rates and the financial burden associated with severe sepsis. It will be important to explore if a simple measure like early administration of appropriate antibiotics decreases hospital length of stay (LOS) and related health care costs. The study will able to assess whether early administration of antibiotics improves patient outcomes and thus establish a better antibiotic protocol in ICU.
Materials and methods:
- Study Setting
- The study will be conducted at AMRI Hospital, Dhakuria, Gariahat Road, Kolkata- 700029.
- Study Design
- This is a prospective observational cohort study.
- Study Duration
- Patients will be observed during the study period commencing from 1stJuly, 2020 to 31st March 2021.
- Study Population
- The study was conducted with all consecutive adult (≥ 18 years of age) patients admitted with a suspected sepsis in the ICU during the study period.
- Inclusion Criteria
- All patients admitted to the ICU during the study period with diagnosis of Sepsis and Septic shock and receiving empirical antibiotics within one hour.
- Exclusion Criteria
- Patients not receiving antibiotics in the ICU.
- Patients receiving antibiotics for surgical prophylaxis.
- Definition
- Sepsis and Septic shock - is defined as per the Sepsis 3 definition.
Sepsis is defined as life-threatening organ dysfunction due to a dysregulated host response to infection.
- Clinical criteria for Sepsis according to sepsis 3 definition:
- Organ dysfunction is defined as an increase of 2 points or more in the SOFA score.
- Patients with suspected infection who are likely to have a prolonged ICU stay or to die in the hospital can be promptly identified at the bedside with qSOFA (“HAT”); i.e. 2 or more of:
- Hypotension: SBP less than or equal to 100 mmHg;
- Altered mental status (any GCS less than 15);
- Tachypnoea: RR greater than or equal to 22.
Septic Shock - Septic shock is a subset of sepsis in which underlying circulatory and cellular/ metabolic abnormalities are profound enough to substantially increase mortality.
- Clinical criteria for septic shock according to sepsis 3 definition:
- Persistent hypotension requiring vasopressors to maintain MAP greater than or equal to 65 mmHg.
- Lactate greater than or equal to 2 mmol/l.
- Study Methods
- Timing of ICU admission - time noted from the patient’s ICU nursing chart when the first vital parameters are noted by the nurse.
- Timing of administration of 1st dose of antibiotic will be noted from ICU nursing chart ( in minutes from the timing of ICU admission ).
- Antibiotic that is administered within the first one hour of admission will be noted from ICU nursing chart.
- Appropriateness of antibiotic - will be assessed from the microbiology culture and sensitivity results once available.
- Outcome measures - will be noted from the ICU database.
- Data will be then recorded systemically in the data collection form and finally entered in the excel sheet for analysis.
- All the data will be then analysed by statistician by appropriate statistical tests.
- Variables
- Variables that will be collected: Patient demographics (age, sex, type of admission (medical or surgical), source of admission, APACHE IV score, co-morbidities, choice of antimicrobials use and actual time of initial parenteral antibiotic (empirical or documented) administration.
- The time of initiation of effective antimicrobial therapy will also be documented.
- The ICU and hospital discharge status, ICU and hospital length of stay and requirement of ICU support (mechanical ventilation, dialysis, vasopressor support) was noted.
- Vitals that were recorded will include the mean values in 1st hour -Systolic BP, heart rate, respiratory rate and mean arterial pressure (MAP). Laboratory parameters that were collected included creatinine, lactate, CRP, INR, platelets
and bilirubin. Statistical analysis was done using appropriate statistical tests on SPSS software.
- Ethical Approval
- Ethical approval was taken from the AMRI Ethics Committee prior to data collection process.
- Statistical Analysis
Descriptive statistics was described as means and standard deviation, frequencies and percentages. Student’s t tests were used to assess the difference between means and Chi square tests were used to determine differences between categorical variables. P<0>
Results:
Baseline Characteristics
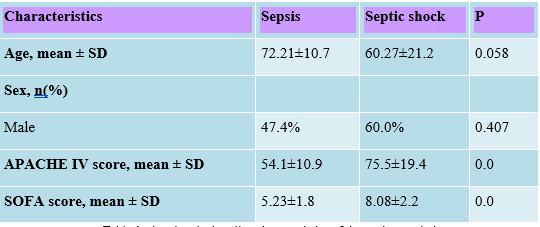
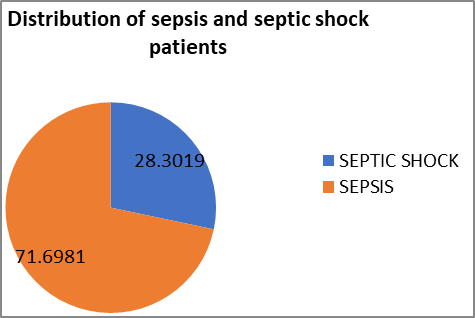
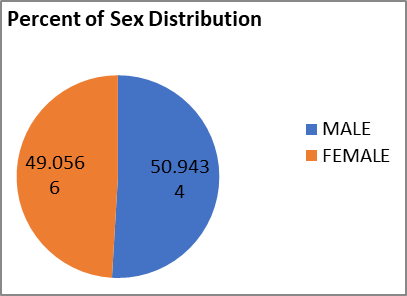
There was a total of 53 patients (n=53) admitted during study period. 71.7% patients were admitted with sepsis and the rest 28.3% with septic shock (Figure 1). Males constituted 50.9% of patients with sepsis and 49.1% of septic shock patients (Figure 2). There was no significant difference in the mean age of patients admitted with sepsis or septic shock (72.21±10.7years vs. 60.27±21.2 years, p=0.058). The mean APACHE IV score of sepsis patients was 54.1 and septic shock was 75.5 and the mean SOFA score of sepsis is 5.23 and septic shock is 8.08. The baseline characteristics of the study population are described in Table 1.
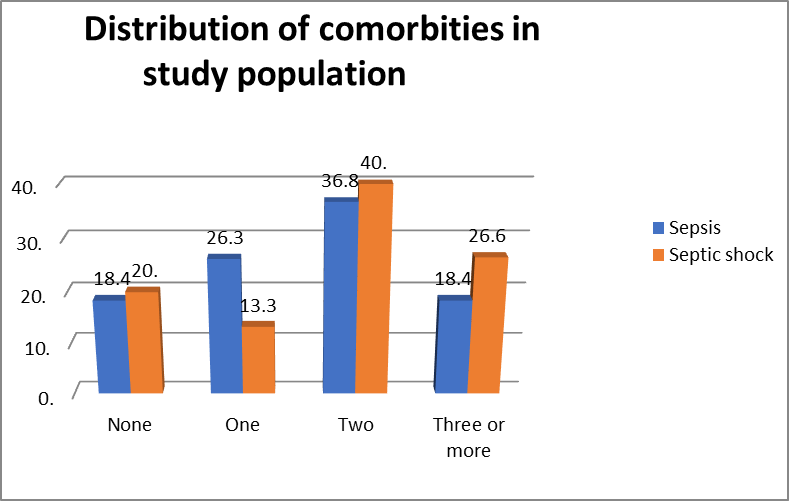
Co-morbidities:
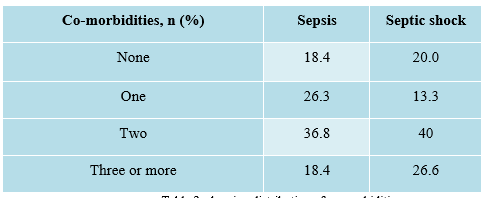
There was no significant difference in the distribution of co-morbidities between the two groups. Majority of patients in both groups had two co-morbidities - 36.8% in sepsis group and 40.0% of patients in the septic shock group. The distribution of co-morbidities is highlighted below in Table 2, Figure 3.
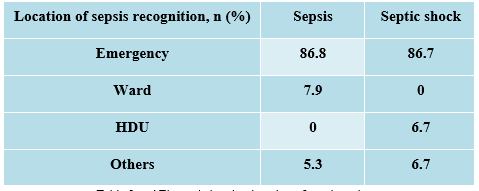
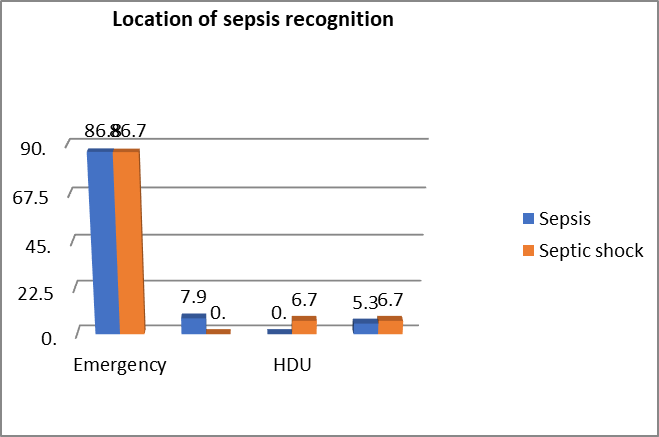
Location of sepsis recognition:
Majority of patients were identified at the emergency (86.8% vs. 86.7% in sepsis and septic shock) followed by ward (7.9% vs. 0% respectively).
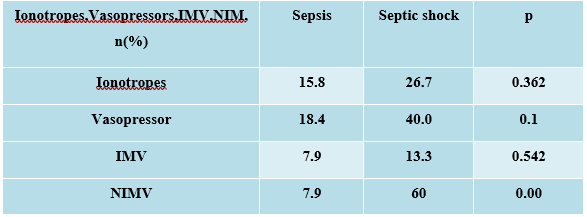
Requirement of inotropes, vasopressor, IMV and NIMV:
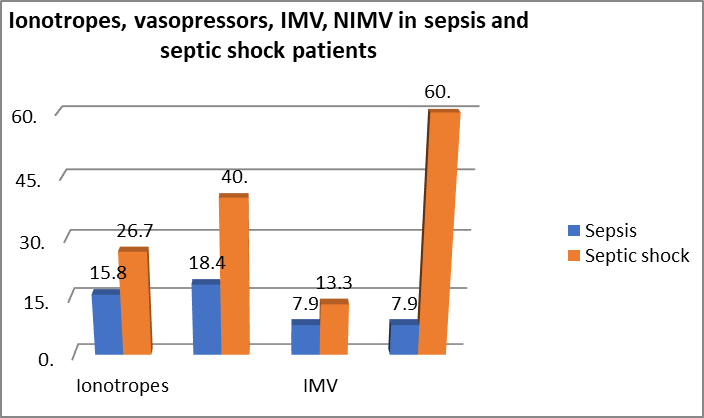
More septic shock patients required inotropes, vasopressors, IMV (Invasive mechanical ventilation), NIMV (Non invasive mechanical ventilation) support compared to sepsis patients (26.7% vs.15.8%, p=0.362; 40% vs.18.4%, p=0.1; 13.3% vs 7.9, p=0.542; and 60% vs 7.9, p=0.00; respectively).
Baseline physiological and laboratory parameters
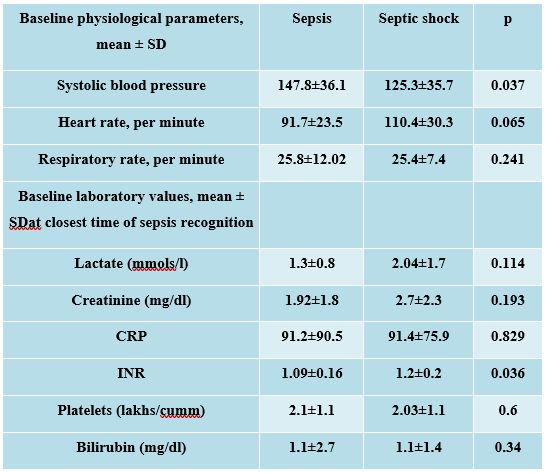
The systolic blood pressure was significantly lower in the septic shock group compared to sepsis group (125.3±35.7 vs 147.8±36.1, p=0.037). There was no major difference in the respiratory rate and diastolic blood pressure between groups. Blood lactate, INR and serum creatinine were higher in septic shock group compared to sepsis group (Lactate: 2.0±1.7mmols/l vs. 1.3±0.8mmols/l, p=0.114; INR: 1.09+ 0.06 vs 1.2+ 0.2, p=0.034, Creatinine: 2.7±2.3mg/dl vs. 1.92±1.8mg/dl) but only the difference in INR was found be statistically significant. There was no difference in the CRP, bilirubin and platelet values between groups (Table 5).
Compliance with initial resuscitation goals:
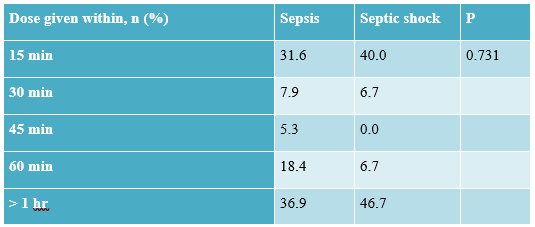
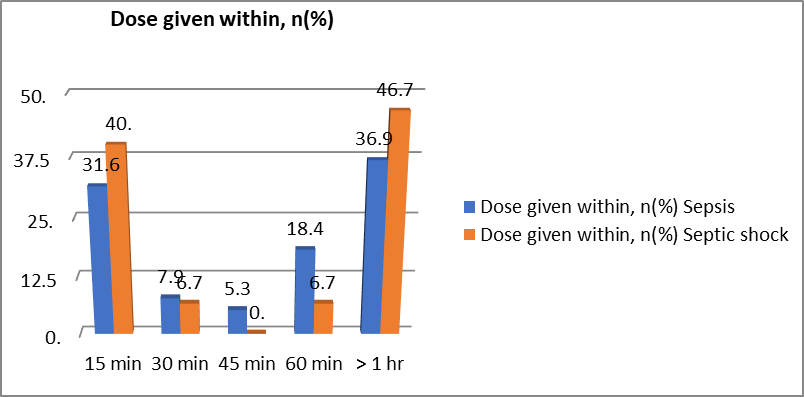
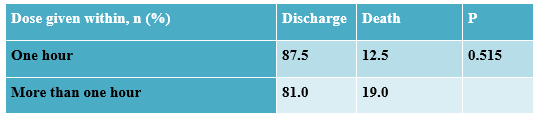
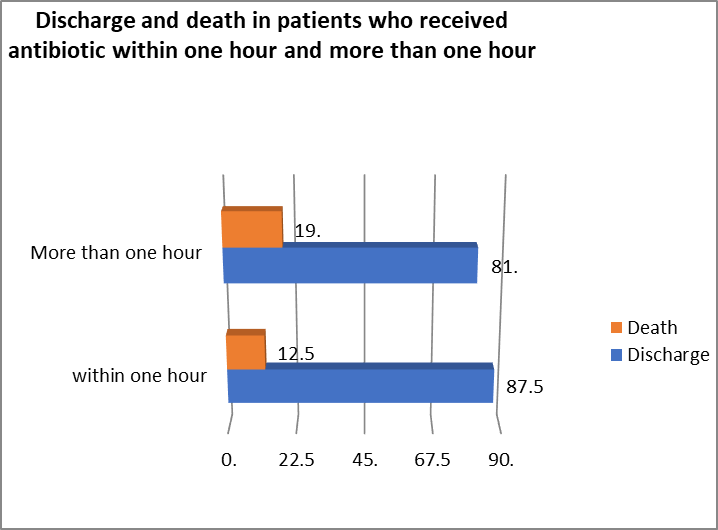
63.2% in the sepsis group and 53.4%% in the septic shock group received antibiotics within the first hour. There was no significant difference in surviving sepsis protocol compliance between the two groups (Table 6, Figure 6).
87.5 % patients who received antibiotic within one hour of admission were discharged compared to 81.0% patients who received first dose of antibiotic beyond one hour of admission (87.5% vs 81.0%, p= 0.515).
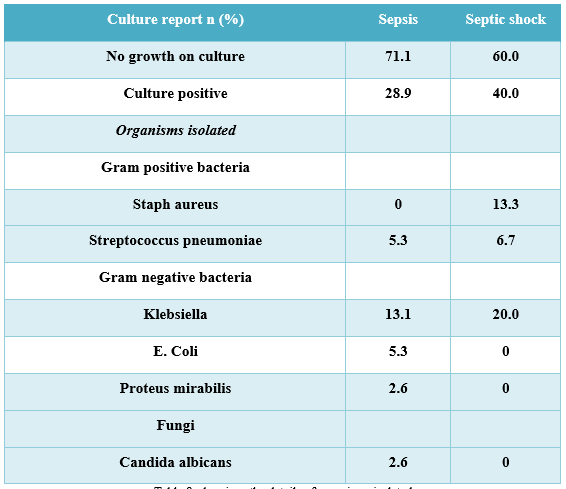
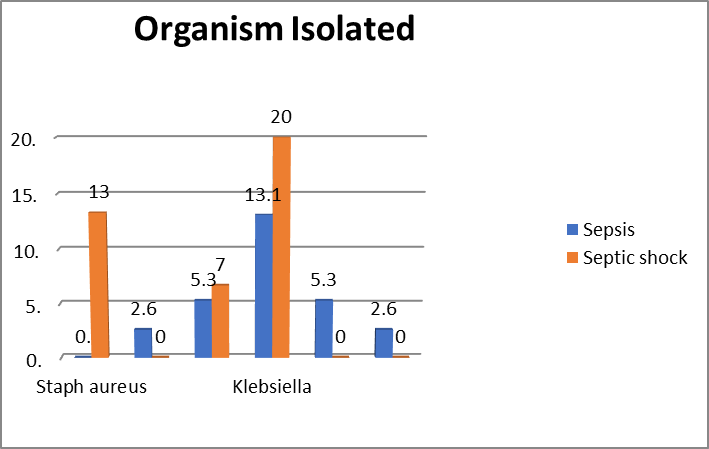
Bacteriology and culture positivity:
Culture positivity was seen only in 28.9% of patients with sepsis and 40.0% of patients with septic shock. Majority of the isolates were gram negative organisms. Gram positive organisms were isolated only in 7.9% of patients with sepsis. The commonest gram-negative organisms were E. coli and Klebsiella in both groups (sepsis 5.3% and 13.1% and septic shock 0% and 20% respectively). (Table 8, Figure 7).
Antibiotic administration details:
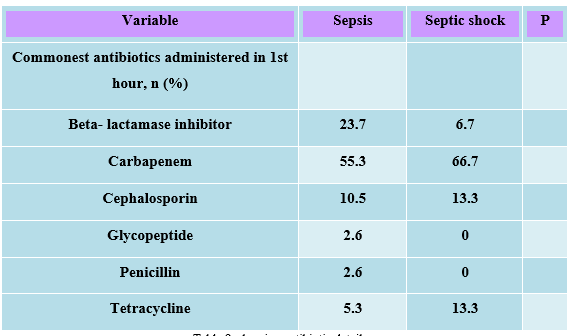
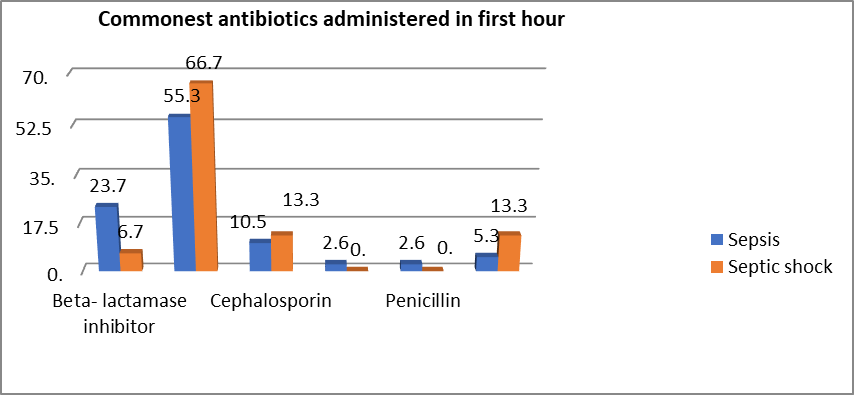
The commonest antibiotic administered was Meropenem in both groups (sepsis: 55.3 %and septic shock: 66.7%) (Table 9, Figure 9).
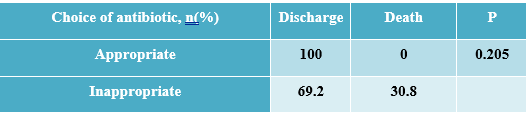
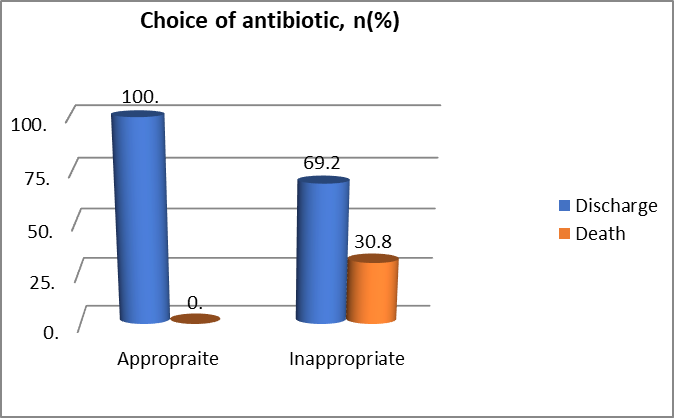
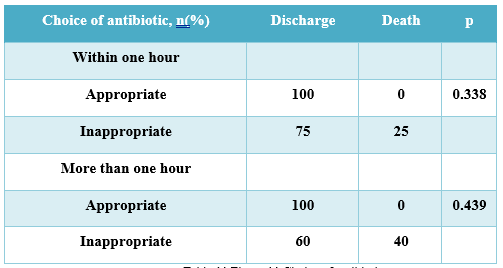
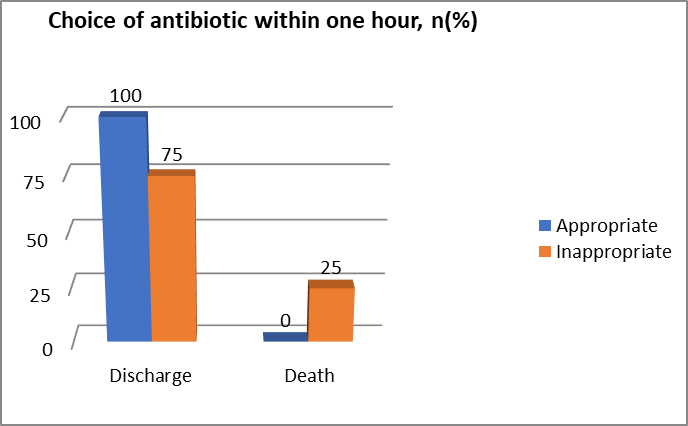
100% patients whose initial antibiotic choice was appropriate were discharged as compared to only 69.2% who received an inappropriate antibiotic empirically. In the group who received the initial appropriate antibiotic, no patient died as compared to a mortality of 30.8% if the initial choice of antibiotic was inappropriate.
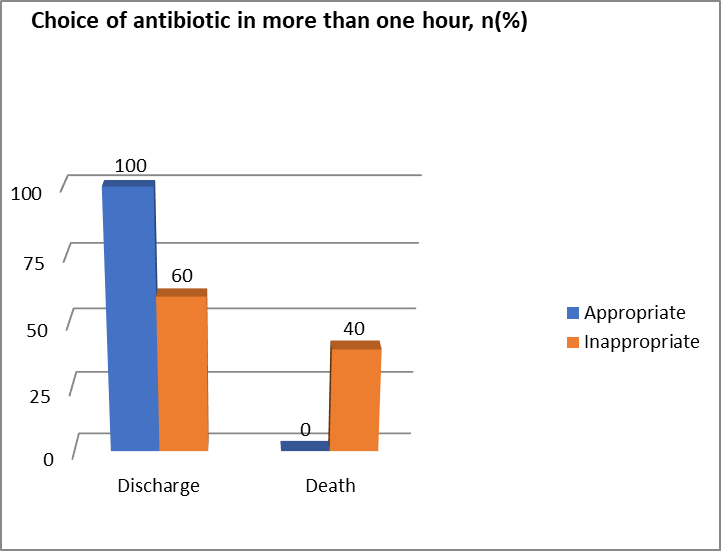
100% patients were discharged who received appropriate antibiotic within one hour or more than one hour whereas 25% patients were died who received inappropriate within one hour and 40% patients were died who received inappropriate antibiotic in more than one hour.
Icu outcome:
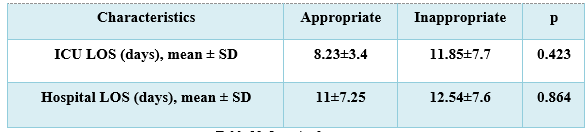
There was no significant difference in the mean ICU length of stay and mean hospital length of stay of patients who received appropriate antibiotic and inappropriate antibiotic (8.23±3.4vs.11.85±7.7, p=0.423; 11±7.25 vs 12.54±7.6, p=0.864 respectively). The baseline characteristics of the study are described in Table 12.
Discussion:
This prospective observational study conducted from February 2021 to April 2021 in AMRI ICUs had included 53 numbers of patients who were ill enough to be admitted in critical care units. Prognosis was assessed by means of APACHE IV and SOFA score in this prospective study. Demographic characteristics of patients, comorbidities, microbiological findings, choice of antimicrobials used, and the actual time of initial parenteral antibiotic(empiric/documented) administration were evaluated. APACHE IV score is a standard scoring system to understand the level of severity of illness and it could be affected by many parameters. Knowing the level of illness is important for treating the patients who needs appropriate care at appropriate time, otherwise the outcome may worsen. There are many studies which looked at use of antibiotics in sicker group of patients like who were in shock stage and their outcome.
In this study mortality was 30.8% in the group whose initial antibiotic choice was inappropriate while no patients died in the group where the patient received appropriate empirical therapy. When appropriateness as well as timing of administration were compared simultaneously, all patients who received appropriate antibiotic within one hour or more than one hour survived to discharge. However, if antibiotic choice was inappropriate, 25% patients died even if they received the antibiotics within one hour and if the first dose was delayed beyond the first hour, the mortality further increased to 40%. Same result was found in study by Kumar et al in 2009.
87.5 % patients who received antibiotic within one hour of admission were discharged compared to 81.0% patients who received first dose of antibiotic beyond one hour of admission (87.5% vs 81.0%, p= 0.515). The fact was also found by P. Naucler et al in 2020.
We found that culture positivity was seen only in 28.9% of patients with sepsis and 40.0% of patients with septic shock. Majority of the isolates were gram negative organisms. Gram positive organisms were isolated only in 7.9% of patients with sepsis. The commonest gram-negative organisms were E. coli and Klebsiella in both groups (sepsis 5.3% and 13.1% and septic shock 0% and 20% respectively). It was also stated in a study by Roberta Capp et all in 2011.
Conclusion
In my study it is demonstrated that gram-negative bacteria remain the major pathogen in sepsis as has been demonstrated in most ICUs in India. Systolic blood pressure was significantly lower and Lactate, INR and creatinine were higher in septic shock group compared to sepsis group. All patients who received appropriate antibiotic were discharged compared with only 69.2% patients discharged whose antibiotic choice was inappropriate. Mortality was 30.8% in the group whose initial antibiotic choice was inappropriate while no patients died in the group where the patient received appropriate empirical therapy. When appropriateness as well as timing of administration were compared simultaneously, all patients who received appropriate antibiotic within one hour or more than one hour survived to discharge. However, if antibiotic choice was inappropriate, 25% patients died even if they received the antibiotics within one hour and if the first dose was delayed beyond the first hour, the mortality further increased to 40%. There was no significant difference in the mean of ICU length of stay and mean hospital length of stay of patients based on appropriateness of empirical antibiotic therapy.
Limitations:
Number of patient population is small due to covid-19 pandemic.
References
- P. Naucler; A. Huttner; C.H. van Werkhoven; M. Singer; P.Tattevin; (2020) et.al Tangden:Impact of time to antibiotic therapy on clinical outcome in patients with bacterial infections in the emergency department: implications for antimicrobial stewardship.Clinical Microbiology and Infection.
View at Publisher | View at Google Scholar - Rational antibiotic utilization in selected pediatric conditions. Malaysian Health Technology Assessment Unit, 2002.
View at Publisher | View at Google Scholar - Gaur AH, (2006) English BK: The judicious use of antibiotics - An investment towards optimised health care. Indian Paediatr, 73, 343-350.
View at Publisher | View at Google Scholar - WHO global strategy for containment of antimicrobial resistance. World Health Organization, 2001.
View at Publisher | View at Google Scholar - Chambers H: Antimicrobial agents: General considerations. Hardman JG, Limbird LE: (2001) The pharmacological basis of therapeutics. New York: MacGraw-Hill, 1143-1169.
View at Publisher | View at Google Scholar - Okeke IN; Aboderin OA; Byarugaba DK; (2007) et al: Growing problem of multidrug-resistance enteric pathogens in Africa. Emerg Infect Dis, 13, 1640-1646.
View at Publisher | View at Google Scholar - Archibald LK, Reiller LB: (2001) Clinical microbiology in developing countries. Emerg Infect Dis, 7, 302-304.
View at Publisher | View at Google Scholar - French GL: Clinical impact and relevance of antibiotic resistance. Adv Drug Deliv Rev, 2005, 57, 1514-1527.
View at Publisher | View at Google Scholar - Davey P; Brown E; Fenelon L; (2005) et al: Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev, (4), CD003543.
View at Publisher | View at Google Scholar - Lodise TP; McKinnon PS; Swiderski L; Rybak M: (2003) Outcomes analysis of delayed antibiotic treatment for hospital-acquired Staphylococcus aureus bacteremia. Clin Infect Dis, 36, 1418-1423.
View at Publisher | View at Google Scholar - Harbarth S; Garbino J; Pugin J; (2003) et al: Inappropriate initial antimicrobial therapy and its effect on survival in a clinical trial of immunomodulating therapy for severe sepsis. Am J Med, 115, 529-535.
View at Publisher | View at Google Scholar - Gonzales R; Bartlett JG; Besser RE; (2001) et al: Principles of appropriate antibiotic use for treatment of non-specific upper respiratory tract infections in adults: background. Ann Intern Med, 134, 490-494.
View at Publisher | View at Google Scholar - Matthias Adorka; MitongaKabwebweHonore; MartieLubbe; Jan Serfontein; Kirk Allen: (2013) The Impact of Appropriate Antibiotic Prescribing on Treatment Evaluation Parameters. J Public Health Africa, 4(1).
View at Publisher | View at Google Scholar - Antimicrobial resistance: Does stopping a course of antibiotics early lead to antibiotic resistance? World Health Organization, 2020
View at Publisher | View at Google Scholar - E Oakley-Hannibal; H Gawda: (2015) G142(P) Are antibiotics administered within one hour in suspected neonatal sepsis as per nice guidelines? British Association of Perinatal Medicine, 100(3).
View at Publisher | View at Google Scholar - Houck PM, Bratzler DW, Nsa W, Ma A, Bartlett JG. (2004) Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med.; 164:637-644.
View at Publisher | View at Google Scholar - Joo YM, Chae MK, Hwang SY, Jin S-C, Lee TR, (2014) et al. Impact of timely antibiotic administration on outcomes in patients with severe sepsis and septic shock in the emergency dept. ClinExpEmerg Med. 1:35-40.
View at Publisher | View at Google Scholar - Buckman, S. A., Turnbull, I. R., & Mazuski, J. E. (2018) Empiric Antibiotics for Sepsis. Surgical Infections, 19(2), 147–154.
View at Publisher | View at Google Scholar - Vilella, A. L., & Seifert, (2006) C. F. Timing and appropriateness of initial antibiotic therapy in newly presenting septic patients. The American Journal of Emergency Medicine, 32(1), 7–13.
View at Publisher | View at Google Scholar - Baré, M., Castells, X., Garcia, A., Riu, M., Comas, M (2006) et.al, Importance of appropriateness of empiric antibiotic therapy on clinical outcomes in intra-abdominal infections. International Journal of Technology Assessment in Health Care, 22(02), 242-248.
View at Publisher | View at Google Scholar - Lancaster, J. W., Lawrence, K. R., Fong, J. J., Doron, S. I., Garpestad, E., (2008) et.al, Impact of an Institution-Specific Hospital-Acquired Pneumonia Protocol on the Appropriateness of Antibiotic Therapy and Patient Outcomes. Pharmacotherapy, 28(7), 852–862.
View at Publisher | View at Google Scholar - Pierre Emmanuel Charles, Claire Tinel, Saber Barbar, SergoAho, SebastienPrin, (2009) et.al, Procalcitonin kinetics within the first days of sepsis: relationship with the appropriateness of antibiotic therapy and the outcome.
View at Publisher | View at Google Scholar - Philip S Stewart, William Costerton: (2001) Antibiotic resistance of bacteria in biofilms. The Lancet, 358(9276), 135-138.
View at Publisher | View at Google Scholar - Roberta Capp, MD; YuchiaoChang, Phd; David F. M. Brown, MD: (2011) Effective Antibiotic Treatment Prescribed by Emergency Physicians in Patients Admitted to the Intensive Care Unit With Severe Sepsis or Septic Shock: Where is the Gap? The Journal of Emergency Medicine, Vol. 41, No. 6, pp. 573–580.
View at Publisher | View at Google Scholar - SurbhiLeekha, MBBS; Christine L. Terrell, MD, Randall S. Edson, MD: (2011) General Principle of Antimicrobial Therapy. Mayo Clinic Proceedings, 86(2), 156-167.
View at Publisher | View at Google Scholar - Christopher J. Grace, MD, FACP; Brad Robinson, MPH, MD: Empiric Antibiotic Selection. Infectious Disease Antimicrobial agents.
View at Publisher | View at Google Scholar - 2Antibiotic Resistance. World Health Organization. 2020.
View at Publisher | View at Google Scholar