Research Article | DOI: https://doi.org/10.58489/2836-6387/005
Effectiveness of Home Based Telerehabilitation for Forward Versus Backward Stepping Strategy in Ground Walking Training on Functional Mobility and Balance Among Spastic Diplegic Cerebral Palsy-- A Simple Experimental Study
1,2 Ph. D Research Scholar, Desh Bhagat University, Mandi Gobindgarh, Punjab, India
3 Professor and Head, Department of Biochemistry, Government Medical College Amritsar, Punjab, India
4 Nursing Officer, Guru Nanak Dev Hospital Amritsar, Punjab, India
*Corresponding Author: Jagroop Singh
Citation: Vijay Kumar Gupta, Jagroop Singh, Dr. Sukhraj Kaur, Manjinder Kaur, (2023). Effectiveness of Home Based Telerehabilitation for Forward Versus Backward Stepping Strategy in Ground Walking Training on Functional Mobility and Balance Among Spastic Diplegic Cerebral Palsy-- A Simple Experimental Study. Journal of Virology and Vaccination. 2(1). DOI: 10.58489/2836-6387/005
Copyright: © 2023 Jagroop Singh, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 12 February 2023 | Accepted: 20 February 2023 | Published: 27 February 2023
Keywords: spastic cerebral palsy; balance; functional mobility; paediatric balance scale
Abstract
Background: The primary focus of physiotherapy interventions for children with CP is to improve locomotor function and functional activities. It is suggested that walking training activates neural circuits that mediate central pattern generators to activate limb muscles repetitively and produced rhythmic movements. Additionally, it adjusts control between agonist and antagonist muscles, leading to enhanced walking speed, and static and functional balance. The purpose of the study is to find out the effectiveness of home based telerehabilitation for forward stepping vs backward stepping strategy in ground walking training on functional mobility and balance among spastic diplegic cerebral palsy.
Methodology: A simple experimental study was conducted on 24 spastic diplegic cerebral palsy who fulfill the selection criteria were selected for this study at the telerehabilitation Unit. A clear explanation was given to every subject and parents/guardian about the procedures and a written consent was obtained from them. Twenty spastic diplegic children were evaluated in person in the department for pre-training and post-training were used as a study design with total study duration was six weeks. (from April 2021 to May 2021). The subjects in group A&B were consisting of 12 subjects and they were treated with home based telerehabilitation for forward and backward ground walking training. Along with that both the group children received routine physiotherapy. Both the groups were received intervention for 15-30 minutes per session, 5 days in a week for a period of 6 weeks. The pre and post score values of balance and functional mobility were measured by using, GMFM walking dimension, modified timed get up and go test and Pediatric Berg balance scale. The values were recorded and documented.
Result: In the statistical analysis of pretest values of both group A and group B were calculated. The pre mean values of PBS for both groups were 33.33 and 33.38. The T-value was 0.3721 the obtained t-value is lesser than the table value and the P-value showed there were no significant in pretest comparison. The posttest mean values of PBS for both groups were 46.08 and 46.33.The T-value was 2.38967,the obtained t-value is greater than the table value. and the P-value showed there were significant in posttest comparison. Alternative hypothesis was accepted. Hence the statistical report states that there were statistically significant differences in posttest comparison. The post score values of the Gross Motor Function Meaure-88, Pediatric Berg Balance Scale and TUG test score in all the variables showed significant difference.
Conclusion: The study concluded that the 6 weeks of backward stepping strategy in ground walking home based telerehabilitation training program along with regular physiotherapy treatment showed statistically significant improvement in balance and functional mobility among spastic diplegic children when compared to forward stepping strategy in ground walking home based telerehabilitation training program.
Introduction
Telerehabilitation [1] is an emerging field as a promising service to reduce the cost of service, to improve access to children with cerebral palsy, to retain patient independence and to facilitate communication between healthcare professionals and the patient in a remote location. The term cerebral palsy [2] describes a group of disorders attributed to non-progressive disturbances that occur in the developing fetal or infant brain and result in a cluster of disorders that impact development of movement and posture, causing activity limitation. The CP children have gait pathologies and tend to lose independent walking at later stages of life because of knee problems, increased spasticity, balance problems, and lack of physical training. Spastic diplegia is one of the most common types of CP in which lower limbs are affected more than upper limbs. Amongst the Spastic CP, Diplegia was present in maximum cases (55%) followed by Quadriplegia 24%, Hemiplegia 19% and Monoplegia 2%. Its incidence in India around 3 cases per 1000 live births; however, being a developing country.
Materials and Methods
A simple experimental study was conducted on 24 spastic diplegic cerebral palsy who fulfill the selection criteria were selected for this study at the telerehabilitation Unit. A clear explanation was given to every subject and parents/guardian about the procedures and a written consent was obtained from them. Twenty spastic diplegic children were evaluated in person in the department for pre-training and post-training were used as a study design with total study duration was six weeks. (from April 2021 to May 2021).
The subjects were included based on the inclusion criteria (both genders with age ranging between 5 to 12 years old, subjects with spastic diplegia cerebral palsy, The Gross Motor Functional Classification System level-II. The exclusion criteria of (all other types of cerebral palsy, Children who cannot participate in the exercise program due to contractures and deformities. Children with cardiac problems like congenital and rheumatic heart diseases. Children who are having visual and hearing deficits).
The Parameters include GMFM – Walking Dimension [3], Balance – Pediatric Berg Balance Scale [4], Functional Mobility – Modified timed get up and go test [5]. The subjects were allocated by into group-A and group-B.
The subjects in group A&B were consisting of 12 subjects and they were treated with home based telerehabilitation for forward and backward ground walking training. Along with that both the group children received routine physiotherapy. Both the groups were received intervention for 15-30 minutes per session, 5 days in a week for a period of 6 weeks. The pre and post score values of balance and functional mobility were measured by using, GMFM walking dimension, modified timed get up and go test and Pediatric Berg balance scale. The values were recorded and documented.
Participant in the Group-A & B childrens are asked or assisted to stand upright in front of Telerehabilitation unit. By starting the ground walking at the lowest speed and gradually increasing to a performance at which the child stepping forward & backward comfortably as tolerated. Physiotherapist instructed and guidance provided to the patient and parents about ground level walking pattern and procedure. A telerehabilitation unit was positioned in front of the patient to provide the child with feedback on postural alignment and to assist motivation. Throughout the program, participants continued with their usual conventional physiotherapy program. The conventional treatment was given for 6 weeks, single session daily. Outcomes were measured on the first and last day of treatment. The conventional treatments were passive, active movements and stretching to both upper, lower limbs and trunk region.
Results
In this study, paired t-test was used to find out the statistical significance between pre and post t-test values of GMFM Score, MTUGT Walking Phase Score, Pediatric Balance Scale Score before and after training for Group A and Group B. The unpaired t-test was used to compare the statistically significance difference of GMFM Score, MTUGT Walking Phase Score, Pediatric Balance Scale Score before and after training for Group A and Group B.
TABLE-I: STATISTICAL ANALYSIS OF GMFM BETWEEN GROUP A & B
TEST | GROUP | MEAN | SD | T-VALUE | P-VALUE |
PRE-TEST | GROUP-A | 71.27 | 4.073 | 0.09111 | >.05 |
GROUP-B | 71.69 | 4.94 | |||
POST TEST | GROUP-A | 79.96 | 3.87 | 6.88407 | <.05 |
GROUP-B | 90.30 | 3.47 |
The statistical analysis of pre test values of both group A and group B were calculated. The pre mean values of GMFM for both groups were 71.27 and 71.69. The T-value was 0.09111the obtained t-value is lesser than the table value and the P-value showed there were no significant pre test comparison. The post test mean values of GMFM for both groups were 79.96 and 90.30. The T-value was 6.88407,the obtained t-value is greater than the table value. and the P-value showed there were significant in post test comparison. Alternative hypothesis was accepted.
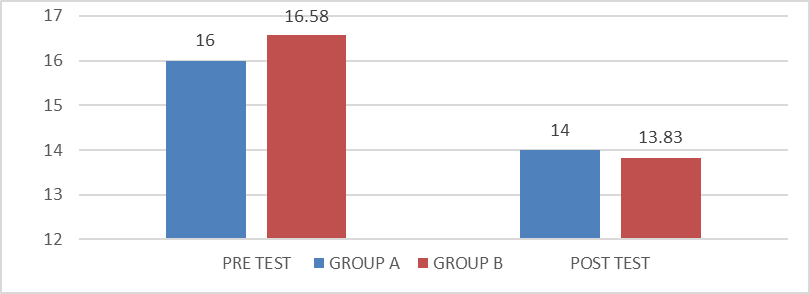
TABLE-II:S TATISTICAL ANALYSIS OF MTUGT BETWEEN GROUP A&B
TEST | GROUP | MEAN | SD | T-VALUE | P-VALUE |
PRE TEST | GROUP-A | 16 | 0.95 | 1.4 | >.05 |
GROUP-B | 16.58 | 1.08 | |||
POST TEST | GROUP-A | 14 | 1.21 | 4.24 | <.05 |
GROUP-B | 13.83 | 1.19 |
In the statistical analysis of pre test values of both group A and group B were calculated. The pre mean values of MTUGT for both groups were 16.00 and 16.58. The T-value was 1.4 the obtained t-value is lesser than the table value and the P-value showed there were no significant in pretest comparison. The posttest mean values of MTUGT for both groups were 14 and 13.83. The T-value was 4.24,the obtained t-value is greater than the table value. and the P-value showed there were significant in post test comparison. Alternative hypothesis was accepted.
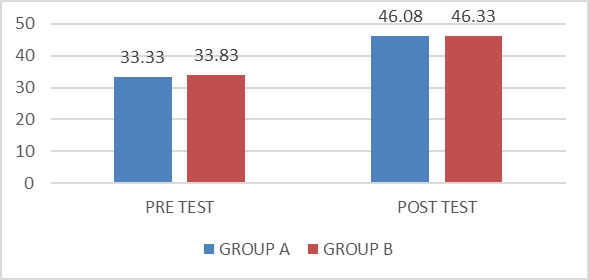
TABLE III: STATISTICAL ANALYSIS OF PBS BETWEEN GROUP A AND GROUP B
TEST | GROUP | MEAN | STANDARD DEVIATION | T-VALUE | P-VALUE |
PRE TEST | GROUP-A | 33.33 | 3.20 | 0.3721 | >.05 |
GROUP-B | 33.83 | 3.38 | |||
POST TEST | GROUP-A | 46.08 | 3.60 | 2.38967 | <.05 |
GROUP-B | 46.33 | 4.68 |
In the statistical analysis of pre test values of both group A and group B were calculated. The pre mean values of PBS for both groups were 33.33 and 33.38. The T-value was 0.3721 the obtained t-value is lesser than the table value and the P-value showed there were no significant in pretest comparison. The posttest mean values of PBS for both groups were 46.08 and 46.33. The T-value was 2.38967,the obtained t-value is greater than the table value. and the P-value showed there were significant in post test comparison. Alternative hypothesis was accepted.
Hence the statistical report states that there were statistically significant differences in posttest comparison. The post score values of the Gross Motor Function Meaure-88, Pediatric Berg Balance Scale and TUG test score in all the variables showed significant difference.
Discussion
This data of the studies emphasized the feasibility and suitability of HBTR to remotely improve of children with functional mobility and balance among spastic diplegic cerebral palsy. Mainly, children with CP were supervised by professionals and adequately monitored through customized technological options. That would be a valuable educational and rehabilitative resource during the current pandemic period. Also, it significantly decreased hospitalization, medical center charges. The pre treatment results may be due to abnormal motor control in children with spastic diplegia. These results were confirmed by Car and shepherd [6], who reported that, the dynamic postural control while walking was impaired in diplegic children due to the following:1- Loss of selective muscle control. 2- Abnormal muscle tone. 3- Relative imbalance between muscle agonists and antagonists across joints,4- Deficient equilibrium reactions. 5-Dependence on primitive reflex patterns for ambulation.
Backward walking acts to improve the patient’s balance and proprioception and will act to condition hip, knee and ankle stabilizers. Both forward walking and backward walking are mediated by the same central pattern generator (CPG), and only small modifications in the CPG are required in order to produce the different characteristics of each walking mode. The reorganization of the muscle synergies or neuromotor control in lower limbs during backward walking might be a possible reason for the improvement of balance by backward walking exercise resulting in more step symmetry while walking [7].
The improvement in the measured parameters can be also attributed to the mechanical and neural responses to backward walking were based on two primary modifications: a reduction in hip movement which probably increases stability by minimizing the anterior-posterior displacement of the center of gravity, and a shorter absolute swing / stance duration. This is supported by the findings of Bobath [8] who reported that hip extension with knee flexion that occurs during backward walking acts to break the extensor synergy of diplegic patients and also the isolated movements of knee alternating flexion with extension were repeatedly practiced in backward walking training and may contribute to improve neuromotor control for patients with diplegia with synergy influence in the lower extremities.
Thus, studies like the present one are important because they compare the walking training in forward & backward directions to verify the impact of each procedure on the ability of locomotion in children with CP. In my present study, subject in control group A were given forward walking ground level training in addition with regular exercise program using home based telerehabilitation unit. Afterwards, subject in experimental group B were given backward walking ground level training in addition with regular exercise program using home based telerehabilitation unit on gross motor function, functional mobility and balance in children with spastic diplegia. The statistical report indicates that there was a significant improvement seen in GMFM score, MTUG score, and PBS after the application of six weeks intervention. So, the backward walking ground level training using home based telerehabilitation unit is the effective treatment technique than forward walking ground level training using home based telerehabilitation to improve gross motor function, functional mobility and balance among subject with spastic diplegic children.
Limitation & Recommendation
The limitations of the study are as follows: Sample size was small, which reduces the generalized ability. Duration of treatment program was only 6 weeks. Only children with limited severity and diagnosis participated in the study. The study assessed only short-term progress of the patient. Long term follow up is needed to evaluate the differences in the condition of the patients from current status. No follow up could be done to determine whether the effect was maintained.
Future study should be done with large sample size with other types and various severities of CP. The same study can be conducted in patients with other neurological disorder such as Spinal cord injury, Cerebrovascular accident, Traumatic brain injury. Further study can be conducted with other GMFCS levels of cerebral palsy to make results more reliable.
Conclusion
The study concluded that the 6 weeks of backward stepping strategy in ground walking home based telerehabilitation training program along with regular physiotherapy treatment showed statistically significant improvement in balance and functional mobility among spastic diplegic children when compared to forward stepping strategy in ground walking home based telerehabilitation training program.
References
- Cano de la Cuerda R, Muñoz-Hellín E, Alguacil- Diego IM, Molina-Rueda F. (2010). Telerehabilitation and neurology Rev Neurol. 2010 Jul 1;51(1):49-56.
View at Publisher | View at Google Scholar - Green MM, Gaebler-Spira D.J Cerebral Palsy. (2019). Pediatr Rehabil Med.12(2):113-114. doi: 10.3233/PRM-190008.
View at Publisher | View at Google Scholar - Jooyeon Ko, Min Young Kim, (2013). Reliability and responsiveness of the gross motor function measure-88 in children with cerebral palsy- Mar;93(3):393-400.
View at Publisher | View at Google Scholar - Lei, Y.; C. Lam; M. Lam et al., (2017). Validity and Reliability of Timed Up and Go Test on Dynamic Balance in 3-5 Years Old Preschool Children. Journal of Yoga and Physical Therapy: 7 (2): 266.
View at Publisher | View at Google Scholar - Franjoine, M. J. Gunther and M. (2003). Taylor Pediatric Balance Scale: a modified version of the Berg Balance Scale for the school-age child with mild to moderate motor impairment. Pediatric Physical Therapy.; 15: 114-128.
View at Publisher | View at Google Scholar - Car and Shepherd: Physical therapy in pediatrics (5th Ed). Butter worth. Heinemann, Oxford: 2008;51
View at Publisher | View at Google Scholar - Van Deursen RW, Flynn TW, Mc Crory JL and Morag E: (1998). Does a single control mechanism exist for both forward and backward walking? Gait & Posture;7
View at Publisher | View at Google Scholar - Bobath B.: Adult hemiplegia evaluation and treatment 3rd edition Oxford utterworth-Heinemann. 1990
View at Publisher | View at Google Scholar - Forward versus backward body weight supported treadmill training on step symmetry in children with spastic diplegia hamada el-sayed abd-allah ayoub. International Journal of Physiotherapy and Research, Int J Physiother Res 2016, Vol 4(5):1639-45.
View at Publisher | View at Google Scholar - Kim, Sung-Gyung; Ryu, Young Uk; Je, Hyun Dong; Jeong, Ji Hoon; Kim, (2013). Hyeong-Dong Backward walking treadmill therapy can improve walking ability in children with spastic cerebral palsy-a pilot study -International Journal of Rehabilitation Research: September 2013 - Volume 36 - Issue 3 - p 246-252
View at Publisher | View at Google Scholar - Amr A Abdel-aziem, Heba MY El-Basatiny Effectiveness of backward walking training on walking ability in children with hemiparetic cerebral palsy: a randomized controlled trial- - Published June 29, 2016
View at Publisher | View at Google Scholar - Stasolla F, Ciarmoli D. (2020). Telerehabilitation to Improve Clinical and Health Conditions of Children with Cerebral Palsy: A Mini Review. Clin Res Psychol; 3(1):1-5.
View at Publisher | View at Google Scholar