Research Article | DOI: https://doi.org/10.58489/2837-3367/005
Decreased Thyroid Function in Nasopharyngeal Carcinoma Patients Who Received Chemoradiotherapy in DR Sardjito Public Hospital, Yogyakarta, Indonesia
1 .Department of Otorhinolaryngology Head and Neck Surgery, Faculty of Medicine, University of Gadjah Mada, Yogyakarta, Indonesia.
*Corresponding Author: Anisa Haqul Khoiria
Citation: Solikin, S. R. Indrasari, A. Surono, A. H. Khoiria, A. Listiati, (2023). Decreased Thyroid Function in Nasopharyngeal Carcinoma Patients Who Received Chemoradiotherapy in DR Sardjito Public Hospital, Yogyakarta, Indonesia. Journal of ENT and Healthcare.2(1). DOI: 10.58489/2837-3367/005
Copyright: © 2023 Anisa Haqul Khoiria, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 13 December 2022 | Accepted: 28 December 2022 | Published: 16 January 2023
Keywords: nasopharyngeal carcinoma, thyroid gland, thyroid function, chemoradiotherapy
Abstract
Background: Radiotherapy has long been recognized as the mainstay for the treatment of nasopharyngeal carcinoma with or without chemotherapy. Chemoradiotherapy can induce a transformation of thyroid gland causing thyroid disorder.
Objective: This study has evaluated a decrease in thyroid function in patients with nasopharyngeal carcinoma who received chemoradiotherapy.
Methods: This is a pre-post study design. The subject includes patients with nasopharyngeal carcinoma that underwent chemoradiotherapy. Patient's thyroid functions were measured twice; before and 3 months after chemoradiotherapy.
Results: We observed the result of 30 patients that underwent chemoradiotherapy. The results of pre and post treatment for FT3, FT4 and TSH show p-value of 0,001, 0,0043 and 0,015 respectively showing statistically significant difference between two measurement period.
Conclusion: We found an alteration in thyroid function in patients with nasopharyngeal carcinoma who received chemoradiotherapy.
Background
Nasopharyngeal carcinoma is the most common malignancy found in Indonesia. It is number ranked fifth amongst malignancy tumor and first amongst head and neck malignancy in Indonesia. It arises from rosenmuller fossa, a transitional area of epithelial mucosal layer, changing from cuboid to squamous epithelium [1,2]. National Comprehensive Cancer Network (NCCN) recommends radiotherapy as the main treatment in nasopharyngeal carcinoma with, or without chemotherapy combination [3].
Radiotherapy for nasopharynx carcinoma can cause disturbance in thyroid gland function, including hypothyroid, thyroiditis, and thyroid nodule. Hypothyroid is a common adverse effect from radiotherapy, contributing 19-53% of cases in head and neck. Post radiotherapy hypothyroid in head and neck cancer mechanism remains unclear. It is associated with small vessel and cell damage, with capsule fibrosis of thyroid gland. Small vessel damage can cause cell degeneration which lead to necrosis and fibrosis. [4,5,6] Fujiwara et al suggested that thyroid gland receiving radiotherapy dosage less than 30 Gray developed less risk of hypothyroid compared to those receiving more than 30 Gray. Furthermore, a study by Lin et al. (2011) on 65 nasopharyngeal cancer patients undergo IMRT, found a change in thyroid gland function in patients receiving radiotherapy with >50 Gray dose [5,6].
Radiation-induced-hypothyroid might affect patient’s quality of life and could be treated with thyroid hormone replacement using levothyroxine, starting from 1,6 µg/kg/day. Thyroid function evaluation is conducted regularly every 3 months after radiotherapy in the first year, and every 6 months in the second to fifth years. Radiation induced hypothyroid incidence can be lowered by reducing radiation volume or by reducing radiotherapy area [6].
Study Aim
This study aims to understand the decrease in thyroid function in patients with nasopharyngeal carcinoma who received chemoradiotherapy
Methods
This is a pre-posttest study design encompassing thirty subjects who were admitted with inclusion criteria of agree to participate in the study by giving written informed consent, diagnosed with nasopharyngeal carcinoma confirmed by histopathology examination, patients were subjected to chemoradiotherapy. Patient who received thyroid hormone therapy, history of radiotherapy in head and neck area either with or without chemotherapy, history of thyroid, hypophyseal, or hypothalamus surgery, patients with thyroid gland tumor and patients receiving thyroid hormone therapy were excluded from this study.
This study was conducted at DR Sardjito Public Hospital, Yogyakarta, Indonesia from January to December 2021. Subjects had received IMRT radiotherapy with average dose of 70 Gray divided into 5 fraction per week, 1 fraction daily. Radiation was given for 45 days; chemotherapy was given concurrently. Analysis was not conducted for chemotherapy. Evaluation of thyroid function using FT3, FT4, and TSH were measured before and three months after chemoradiotherapy. The same measuring instrument was used to process the sample in the clinical pathology laboratory at DR Sardjito Public Hospital.
TSH was observed using chemiluminescent method, with normal value 0,27-4,20 μIU/mL. FT4 was observed using chemiluminescence immunoassay (CLIA), with normal value 1,00-1,70 ng/dL. FT3 was observed using electrochemiluminescence (ECL), with normal value 2,60-4,40 pg/mL. The data then analysed using paired t-test, or using Wilcoxon test if requirement is not met. Fisher exact test was used to evaluate each variable. This study had received ethical approval from Medical and Health Research Ethics Committee (MHREC) Faculty of Medicine, Public Health, and Nursing University of Gadjah Mada with registration number of KE/FK/0078/EC/2021.
Results And Discussions
Thirty nasopharynx carcinoma patients who received chemoradiotherapy were included in this study. Mean age was 48,33 years old. Mean radiation dose was 7065,3 cGray and mean radiation single dose was 214,1 cGray.
Table 1. Characteristics of patients
Variable | Minimum | Maximum | Mean | Deviation Standard |
Age (years old) | 17 | 69 | 48.33 | 11.18 |
Total radiation dose (cGray) | 6864 | 7293 | 7065.3 | 96.64 |
Single radiation dose (cGray) | 208 | 221 | 214.1 | 2.93 |
Pre FT3 (pg/mL) | 2.24 | 5.10 | 3.20 | 0.73 |
Post FT3 (pg/mL) | 1.53 | 5 | 2.63 | 0.62 |
Pre FT4 (ng/dL) | 0.55 | 2.01 | 1.25 | 0.30 |
Post FT4 (ng/dL) | 0.81 | 1.48 | 1.12 | 0.18 |
Pre TSH (µIU/mL) | 0.04 | 5.66 | 1.61 | 1.20 |
Post TSH (µIU/mL) | 0.06 | 11.45 | 2.41 | 2.35 |
Majority of patients in this study were 30-60 years old (83,3%), only 10% were > 60 years old, and 6,7% were < 30>et al. (2018) that mentioned the mean age for patients were 48,1 years old [7]. Other study the mean age for patients was 49,9 ± 12,9 years old and were mostly found between 30-60 years old. Seventy percent of the subject were male (70%) [8,9]. Similar findings in his study with 78 male subject and 11 female subjects. Based on tumor stage, T1-T2 stage contributed to 60% compared to T3-T4 which contributed to 40%. This finding supports previousfindings in which T2 stage were found in 140 subjects [10,11]. T1-T2 stage had post-radiotherapy hypothyroid more than T3-T4 stage (P=0,044) [12]. Another research reported that out of 10 T1-T2 subjects, 7 of them showed post-radiotherapy hypothyroid [13].
Table 2. Frequency Distribution
Variable | Total | Percentage (%) |
Age |
|
|
<30> 30-60 years old >60 years old | 2 | 6.7 |
25 | 83.3 | |
3 | 10 | |
Gender |
|
|
Male Female | 21 | 70 |
9 | 30 | |
T |
|
|
T1-T2 T3-T4 | 18 | 60 |
12 | 40 | |
N |
|
|
N0-N1 N2 N3 | 17 | 56.7 |
9 | 30 | |
4 | 13.3 | |
Stage |
|
|
I-II III-IV | 10 | 33.3 |
20 | 66.7 | |
Radiation Technique IMRT |
|
|
30 | 100 | |
FT3 Difference Decrease Not Decrease |
|
|
23 | 76.7 | |
7 | 23.3 | |
FT4 Difference Decrease Not Decrease |
|
|
20 | 66.7 | |
10 | 33.3 | |
TSH Difference Decrease Not Decrease |
|
|
22 | 73.3 | |
8 | 26.7 |
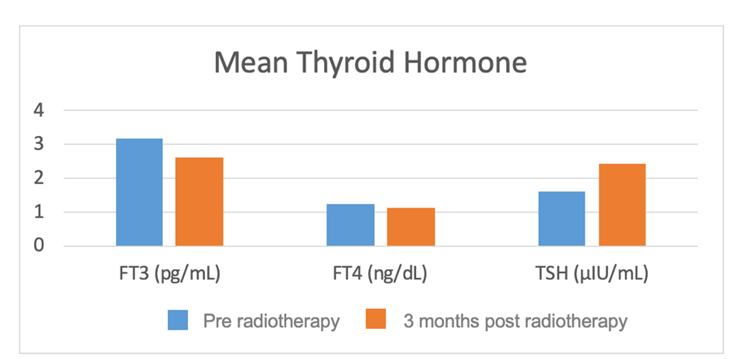
Figure 1. showed mean thyroid function before and 3 months after radiotherapy only. FT3 (pg/mL) level decreased from 3.2±0.72 to 2.63±0.61, FT4 (ng/dL) level decreased from 1.25±0.29 to 1.12±0.17, and TSH (µIU/mL) increased from 1.61±1.19 to 2.42±2.35. Figure 1. Also showed difference between FT3, FT4, and TSH level evaluated pre and post chemoradiotherapy were significant.
Table 3. Paired t-test
Variable | Pre | Post | p-value |
FT3 (pg/mL) | 3.2±0.72 | 2.63±0.61 | 0.001** |
FT4 (ng/dL) | 1.25±0.29 | 1.12±0.17 | 0.043* |
TSH (µIU/mL) | 1.61±1.19 | 2.42±2.35 | 0.015** |
*Paired t-test p<0>
Among nasopharyngeal carcinoma patient who established cervical lymph node metastasis, radiotherapy usually covered more than 75% of all lymph nodes in the neck, promoting risk of thyroid dysfunction after radiotherapy.13 Hypothyroid usually occur at the first 2 years after radiotherapy. The increase dose exposure on thyroid gland will shorten its latency period [13,14]. Miller and Agrawal. (2019) stated that the early hypothyroid sign can be observed 4-6 weeks after treatment completion [13,14]. Lin et al. (2018) reported the decrease of average amount FT4 from 13,1 pmol/L to 10,3 pmol/ in 30 months (-23,5%) and become relatively more stable after 36 months (10,7 pmol/L) after radiotherapy. Meanwhile, mean TSH level increased gradually after radiotherapy, peaking around 24 months, and remained stable after 36 months. Other study also reported decrease in FT3 from 4,87 pmol/L to 4,77 pmol/L on 6 months after radiotherapy, FT4 level also decrease from 16,73 pmol/L to 14,16 pmol/L. TSH level were reportedly increased 21,3% 3-6 months after radiotherapy [13,14]. This study found decrease in thyroid function 3 months after chemoradiotherapy.
The derivation in thyroid function was associated with cell and small vasculature damage of thyroid glands, also with fibrosis of thyroid capsule. These damages generate cell degeneration leading to necrosis and fibrosis. Observation using electron microscope on blood vessels after radiotherapy showed fibrosis on the blood vessel’s wall and narrowing of the lumen. This reduction in lumen size caused hypoxemia, decreasing nutritional supply, and synthesis capacity [14,15]. Another hypothesis estimated that there were increased abnormal thyroid antibodies in nasopharyngeal carcinoma patients who received radiotherapy, thyro-peroxidase antibody (anti-TPO) and thyroglobulin antibody (anti-TG). After high dose radiation, there will be an inflammation of thyroid gland that induce anti-TPO production.
Anti TPO would impair TPO enzyme and hinder thyroid hormones production, leading to hypothyroid. [15,16]. Previous study reported 11,1% subclinical hypothyroid and 31,1% clinical hypothyroid found 9 months after radiotherapy. Radiation dosage greater than 40 Gray will increase the risk of hypothyroid. According to Fujiwara et al. (2014), thyroid glands that received <30>30 Gray. Radiation dose greater than 2,25 Gray will induced thyroid gland follicular cell death through apoptosis. Different study suggests that hypothyroid will increase when thyroid gland was given >45 Gray radiation [16]. Similar study showed that mean dose at <50>
This study had its limitations, such as limited control on factors that can influence thyroid hormone function. This study only measure thyroid function 3 month after chemoradiotherapy. Further evaluation of thyroid function should be done periodically until 24 months after radiotherapy to understand the pattern of thyroid function deflation.
Conclusion
This study demonstrates decreased in thyroid function in nasopharyngeal carcinoma patients who received chemoradiotherapy.
References
- Ghoncheh, M., Mahdavifar, N., Darvishi, E., Salehiniya, H (2016). Epidemiology, incidence and mortality of breast cancer in Asia. Asian Pacific J. Cancer Prev;7(6): 47–52. doi:10.7314/APJCP.2016.17.S3.47
View at Publisher | View at Google Scholar - Chuang, W.Y., Chang, S.H., Yu, W.H., Yang, C.K., Yeh, C.J. (2020), et al. Successful identification of nasopharyngeal carcinoma in nasopharyngeal biopsies using deep learning. Cancers (Basel); 12(1). doi:10.3390/cancers12020507
View at Publisher | View at Google Scholar - Pfister, D.G., Spencer, S., Adelstein, D., Adkins, D., Anzai, Y. (2020), et al. Head and neck cancers,version 2.2020. JNCCN J. Natl. Compr. Cancer Netw; 18(1): 873–898. doi:10.6004/jnccn.2020.0031
View at Publisher | View at Google Scholar - Miller, M.C., Agrawal, A (2009). Hypothyroidism in postradiation head and neck cancer patients: Incidence, complications, and management. Curr. Opin. Otolaryngol. Head Neck Surg; 17(1): 111–115. doi:10.1097/MOO.0b013e328325a538
View at Publisher | View at Google Scholar - Lin, Z., Wu, V.W.C., Lin, J., Feng, H., Chen, L (2011). A longitudinal study on the radiation-induced thyroid gland changes after external beam radiotherapy of nasopharyngeal carcinoma. Thyroid; 21(1): 19–23. doi:10.1089/thy.2010.0229
View at Publisher | View at Google Scholar - Kim, M.Y., Yu, T., Wu, H.G (2011). Dose-volumetric parameters for predicting hypothyroidism after radiotherapy for head and neck cancer. Jpn. J. Clin. Oncol; 44(1): 331–337. doi:10.1093/jjco/hyt235
View at Publisher | View at Google Scholar - Fujiwara, M., Kamikonya, N., Odawara, S., Suzuki, H., Niwa, Y. (2014), et al. The threshold of hypothyroidism after radiation therapy for head and neck cancer: A retrospective analysis of 116 cases. J. Radiat. Res; 56(3): 577–582. doi:10.1093/jrr/rrv006
View at Publisher | View at Google Scholar - Lin, Z., Wang, X., Xie, W., Yang, Z., Che, K., Wu, V.W (2013). Evaluation of clinical hypothyroidism risk due to irradiation of thyroid and pituitary glands in radiotherapy of nasopharyngeal cancer patients. J. Med. Imaging Radiat. Onco; 57(2): 713–718. doi:10.1111/1754-9485.12074
View at Publisher | View at Google Scholar - Huang, C.L., Tan, H.W., Guo, R., Zhang, Y., Peng, H. (2019), et al. Thyroid dose-volume thresholds for the risk of radiation-related hypothyroidism in nasopharyngeal carcinoma treated with intensity-modulated radiotherapy—A single-institution study. Cancer Med; 8(1): 6887–6893. doi:10.1002/cam4.2574
View at Publisher | View at Google Scholar - Xu, Y., Shao, Z., Tang, T., Liu, G., Yao, Y. (2018), et al. A dosimetric study on radiation-induced hypothyroidism following intensity-modulated radiotherapy in patients with nasopharyngeal carcinoma. Oncol. Lett;16(1): 6126–6132. doi:10.3892/ol.2018.9332
View at Publisher | View at Google Scholar - Murthy, V., Narang, K., Ghosh-Laskar, S., Gupta, T., Budrukkar, A., Agrawal, J.P (2014). Hypothyroidism after 3-dimensional conformal radiotherapy and intensity-modulated radiotherapy for head and neck cancers: Prospective data from 2 randomized controlled trials. Head Neck; 36(1): 1573–1580. doi:10.1002/hed.23482
View at Publisher | View at Google Scholar - Wu, Y.H., Wang, H.M., Chen, H.H.W., Lin, C.Y., Chen, E.Y.C. (2010), et al. Hypothyroidism After Radiotherapy for Nasopharyngeal Cancer Patients. Int. J. Radiat. Oncol. Biol. Phys.; 76(4): 1133–1139. doi:10.1016/j.ijrobp.2009.03.011
View at Publisher | View at Google Scholar - Lin, Z., Yang, Z., He, B., Wang, D., Gao, X. (2018), et al. Pattern of radiation-induced thyroid gland changes in nasopharyngeal carcinoma patients in 48 months after radiotherapy. PLoS One; 13(7): 1–9. doi:10.1371/journal.pone.0200310
View at Publisher | View at Google Scholar - Leoncini, E., Ricciardi, W., Cadoni, G., Arzani, D., Petrelli, L. (2014), et al. Adult height and head and neck cancer: A pooled analysis within the INHANCE Consortium. Head Neck; 36(1): 1391. doi:10.1002/hed.23482
View at Publisher | View at Google Scholar - Srikantia, N., Rishi, K.S., Janaki, M.G., Bilimagga, R.S., Ponni, A. (2011), et al. How common is hypothyroidism after external radiotherapy to neck in head and neck cancer patients? Indian J. Med. Paediatr. Oncol; 32(3): 143–148. doi:10.4103/0971-5851.92813
View at Publisher | View at Google Scholar - Bhandare, N., Kennedy, L., Malyapa, R.S., Morris, C.G., Mendenhall, W.M (2007). Primary and Central Hypothyroidism After Radiotherapy for Head-and-Neck Tumors. Int. J. Radiat. Oncol. Biol. Phys.; 68(4): 1131–1139.
View at Publisher | View at Google Scholar