Case Report | DOI: https://doi.org/10.58489/2836-5917/017
Co-Existence of Sickle Cell Disease with Rheumatic Heart Disease
1 PG Resident Hamdard Institute of Medical Sciences & Research (HIMSR) Jamia Hamdard University, New Delhi – 110062
2,3 Department of Medicine, Hamdard Institute of Medical Sciences & Research (HIMSR) Jamia Hamdard University New Delhi – 110062
4 Department of Medicine, Hamdard Institute of Medical Sciences & Research (HIMSR) Jamia Hamdard University New Delhi – 110062
*Corresponding Author: Ruchi Sharma*,
Citation: Ruchi Sharma, (2024). Co-existence of Sickle Cell Disease with Rheumatic Heart Disease. – A Case Report. Clinical Cardiovascular Research. 3(1); DOI: 10.58489/2836-5917/017
Copyright: © 2024 Ruchi Sharma, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 17 February 2023 | Accepted: 14 April 2023 | Published: 13 March 2024
Keywords: sickle cell disease; rheumatic heart disease; 2-D echocardiography; anemia; cardiovascular examination
Abstract
Sickle Cell Disease (SCD) is common in some part of India especially area inhabited by the Dravidian Tribal Population. Co-existence of Sickle Cell Disease with Rheumatic Heart Disease is not uncommon. The clinical findings in sickle cell anemia closely simulate those of rheumatic heart disease. This poses an important diagnostic challenge for the clinicians. Availability of 2-D Echocardiography has made it simpler to diagnose rheumatic heart disease in patients with sickle cell anemia whenever there is mixed symptoms & signs in a patient. We hereby report a case of Sickle Cell Disease with Rheumatic Heart Disease.
Case Report
An Eighteen years female, native of the State of Chhattisgarh of India, presented to the Outpatient Clinic with chief complaints of pain in the entire back & shortness of breath for 2 days. The patient was apparently well 2 days back when she developed pain in the left shoulder gradually involving the whole back, squeezing in nature. She consulted General Practitioner, who advised her pain killers, however, the pain was not relieved. The patient had persistent pain, so she was hospitalized.
The next day of admission, the patient-reported left elbow pain, gradual in onset and associated with swelling over the left elbow joint, which was relieved with medication.
The patient developed jaundice and yellow discoloration of urine a day after admission. Past history revealed episodes of elbow & ankle joint swelling with pain, chest and back pain on and off for the past 10 years. She also gave the history of sore throat on and off for the last 8 years. She gave a history of bleeding from the nose on and off for the past 2 years.
Family history revealed both parents being healthy. The patient has four siblings. The younger brother had similar episodes of joint pain, body ache and jaundice and died at the age of 7 years due to weak liver as informed by the treating doctor.
On clinical examination, she was conscious, oriented, and well-hydrated. She is of a thin build, had pallor, and there was an icteric tint present in the conjunctiva. No clubbing or lymphadenopathy was found. Her JVP was normal, her Pulse was 92 beats/min., and her Blood pressure in her right arm was 110/70 mm Hg.
Cardiovascular Examination revealed normal precordium on inspection. Apex beat present at 5th intercostal space at the anterior clavicular line. There were no visible precordial pulsations. Apex beat on palpation was tapping type, mild precordial heave present & no epigastric pulsations noted. No palpable thrill were found. On percussion, there was normal cardiac dullness. On auscultation first heart sound (S1) was loud. There was grade 3/6 Mid diastolic murmur at apex, localized with no radiation. There was grade 2/6 Mid systolic murmur, heard at apex, non-radiating. There was mid systolic click & Pulmonic component of second heart sound (P2) was loud.
On Abdominal examination, the liver was palpable, 3 cm below the costal margin & tender. Splenomegaly was present. Respiratory system and neurological examination were normal.
In view of the above-mentioned clinical features, a diagnosis of Rheumatic heart disease with anemia was made & the patient was investigated for the same.
Hematological Examination revealed – Hb 8.3 mg/dl (11- 13 mg/dl), TLC was 9. 76 (4.00 – 11.0 x 10 9/ L), neutrophils – 83.8 %, lymphocytes- 11.2%, MCV- 87.3(80 to 100 fl), MCH- 30.1 (27.5 – 33.2 pg), MCHC- 34.4 g/dl (33.4 – 35.5), platelet count – 147 MCL x 10 / L.
Peripheral blood smear exams showed reduced red cell mass, RBC – moderate anisopoikilocytes, predominantly microcytic hypochromic with the presence of few macrocytes, tear drop cells, target cells with elliptocytes (Dimorphic anemia). Total & Differential leukocyte counts were normal, platelets were adequate.
Reticulocyte count was 6.7, Direct and Indirect Coombs test was negative. Viral markers were negative. HPLC was done in which HbA was 9.8% Hb A2 - 2.9%, HbF - 20.4%, HbS- 67%. Serum Haptoglobulin was <0>
Liver Function Test revealed – Total bilirubin – 4.22 mg/dL (0.1 to 1.2 mg/dl), S. Bilirubin (Direct)-0.93 mg/dl (less than 0.3 mg/dl), and Indirect bilirubin- 3.29 mg/dl
Kidney function test revealed blood urea 21.4 (2.5 to 7.1 mmol/L) and serum creatinine was 0.46 mg/dl, (0.84 to 1.21 mg/dl).
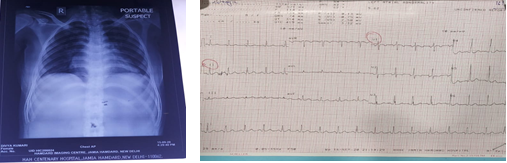
X-ray Chest & ECG were normal (Fig 1 & 2)
2-D ECHO was suggestive of Rheumatic Heart Disease with moderately thickened, Anterior5 mitral leaflet (AML) showed diastole doming, post mitral leaflets (PML) shows restricted motion with mitral valve area of 2.1 cm2. Moderate mitral regurgitation (eccentric jet). There was tricuspid regurgitation. Pulmonary artery systolic pressure was around 40 mm Hg with good right and left ventricular function. There was no pericardial effusion or clot (Fig 3).
A final diagnosis of Rheumatic heart disease with sickle cell anemia was made. The patient was treated with hydroxyl urea & folate supplementation besides a blood transfusion. She improved clinically and was discharged with advice to continue the above-mentioned treatment and Penicillin prophylaxis 1.2 lacs/month for RHD and to remain under regular follow-up.
Discussion
Sickle cell disease is particularly common among people whose ancestors come from sub-Saharan Africa, South America, Cuba, Central America, Saudi Arabia, India, Turkey, Greece, and Italy.
Indian Prevalence
First described in the Nilgiri Hills of Northern Tamil Nadu in 1952, the sickle cell gene is now known to be widespread among people of the Deccan Plateau of Central India with a smaller focus in the North of Kerala and Tamil Nadu. Anthropological survey of India has documented the distribution and frequency of the sickle cell traits which reaches level as high as 35% in some communities especially in tribal population (1, 2).
Haemoglobin S results from a single base mutation in beta chain of haemoglobin, the adenine base is replaced by thymine, so glutamic acid is replaced by valine. The sickling test and haemoglobin electrophoresis help in diagnosis and differentiate homozygous from heterozygous types.
Sickle cell diseases (SCDs) are severe and chronic inflammatory processes on vascular endothelium, terminating with end-organ insufficiencies in early years of life. Haemoglobin S (HbS) causes loss of elasticity and biconcave disc shaped structures of red blood cells (RBCs). Probably loss of elasticity instead of shape is the main problem since sickling is rare in peripheric blood samples of the SCDs with associated thalassemia minors, and human survival is not so affected in hereditary spherocytosis or elliptocytosis. Loss of elasticity is present during whole lifespan, but exaggerated with various stresses of the body. The hard RBCs induced severe and chronic vascular endothelial damage, inflammation, edema, and fibrosis terminate with tissue hypoxia all over the body (3, 4). Capillary systems may mainly be involved in the process due to their distribution function for the hard bodies.
RHD is caused by an autoimmune reaction against Group A b-hemolytic streptococci. The majority of morbidity and mortality associated with rheumatic fever is caused by its destructive effects on cardiac valves. It is characterized by repeated inflammation with fibrinous repair. Fibrosis and scarring of valve leaflets, commissures, and cusps lead to abnormalities that can result in valvular stenosis or regurgitation. The valvular endothelium is a prominent site of lymphocyte-induced damage.
Moderate to severe anemias, auto-splenectomy, frequent painful crises, hospitalizations, invasive procedures, RBC, and a suppressed mood of the body may just be some of the possible reasons of immunosuppression in the SCDs (27-29). As a result, the significantly higher prevalence of RHD due to repeated bacterial infections is not an uncommon finding in the SCDs.
The confusing resemblance between the symptoms of sickle cell anaemia and those of rheumatic heart disease is well known. Yater and Hansmann have pointed out that the diagnosis of rheumatic heart disease in cases of sickle cell anaemia has been made many times from the history of joint pains, presence of an enlarged heart, systolic mitral or precordial murmur, and hepatomegaly. Other common symptoms are leg pain, ankle edema, pallor, and dyspnoea. Often-times organic heart disease is diagnosed clinically only to find at autopsy that all changes noted are compatible with a severe anaemia (3)
Rheumatic heart disease and sickle cell anaemia are frequently diagnosed in the same patient. The differentiation of sickle cell anaemia from rheumatic heart disease with mitral stenosis may be impossible on clinical grounds alone (Bland, White and Jones, McKusick) (4).
Klinefelter has shown that the clinical findings in sickle cell anaemia could closely simulate those of rheumatic heart disease, but noted that specific lesions have never been demonstrated at autopsy. Hansman emphasized the importance of being extremely cautious in making a non-anaemia diagnosis of heart disease when studying a patient with sickle cell anaemia. The clinical discussion as to whether sickle cell anaemia alone is present or whether there is an accompanying rheumatic heart lesion is made even more complex by Cooley’s statement: “Organic heart disease is about as common here (sicklemia) as in any group of children subject to tonsillitis as these children often are.”
Very recent study by Mehmet Rami Helvaci etal’ in 428 patients with the SCDs (208 females) and 2,855 controls (1,620 females), found RHD just in 0.3% of control (eight females and one male). Whereas this was 6.5% (13 females and 15 males) in the SCDs (p<0>
Conclusion
Many of the clinical symptoms and signs of sickle cell disease and rheumatic heart disease are similar in nature. To differentiate these two conditions based on clinical examination is a significant challenge to clinicians. However, meticulous history taking especially probing about the geographic origin of the patient and family history helps in getting clues about the possibility of sickle cell disease in a given patient. Echocardiography remains the gold standard for diagnosing concomitant rheumatic heart disease in a patient with sickle cell disease.
References
- Rohan B Colah (2015) May et al. Sickle cell disease in tribal populations in India. Indian J Med Res 141, 509-515.
View at Publisher | View at Google Scholar - Graham R Serjeant (2016) Jan et al. Sickle cell disease in India: A perspective. Indian J Med Res 143, 21-24.
View at Publisher | View at Google Scholar - EF Bland (1951) et al. Rheumatic Fever and Rheumatic Heart Disease; a twenty-year report on 1000 patients followed since childhood. Circulation 1951, Dec 4(6); 836-843.
View at Publisher | View at Google Scholar - Yater WMH GH. (1936) Sickle-Cell Anemia: A New Cause of Cor Pulmonale: Report of Two Cases with Numerous Disseminated Occlusions of the Small Pulmonary Arteries. American Journal of the Medical Sciences. 191: 474–484.
View at Publisher | View at Google Scholar - Mehmet Rami Helvaci (2020) et al. What a high prevalence of rheumatic heart disease in sickle cell patients. World Family Medicine Journal; 18(8): 74-79.
View at Publisher | View at Google Scholar