Case Report | DOI: https://doi.org/10.58489/2836-5038/010
Adipose-Derived Stem Cell Injection on a Grade III Medial Collateral Ligament Tear in a Soccer Player: A Case Report
1Miami Beach, FL, US · Miami, FL, US · Aventura, FL, US · North Miami Beach, FL, US · Doral, FL, US · Kendall, FL, US
*Corresponding Author: Carlos de la Hoz*
Citation: Carlos de la Hoz, Phillippe Wuilleumier, Amy Riumbau, Carla Cerra. Adipose-Derived Stem Cell Injection on a Grade III Medial Collateral Ligament Tear in a Soccer Player: A Case Report. International Journal of Stem Cells and Medicine.2(1). DOI: 10.58489/2836-5038/010
Copyright: © 2023 Carlos de la Hoz, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 14 February 2023 | Accepted: 27 February 2023 | Published: 18 August 2023
Keywords: Adipose-derived stromal cell, Functional recovery, Medial collateral ligament, Mesenchymal stem cells, Regeneration, Sports injury
Abstract
Stem cells are undifferentiated cells that can divide and differentiate into various types of cells. This special ability makes stem cells a hopeful treatment for regenerating damaged tissue and restoring diminished or completely lost function. In this case study, we discuss a 19-year-old soccer player who presented with a Grade III MCL tear on the right knee. Treatment for a Grade III MCL tear is controversial being that both surgical and non-surgical approaches have been effective. However, due to the patient’s sports background, the patient came to our clinic seeking a faster recovery using a non-surgical treatment. After extensive medical examinations, the patient began a treatment based on adipose tissue-derived stem cells injection. Adipose tissue-derived stem cells were harvested and injected into the distal insertion of the superficial MCL and on the deep MCL origin. After 122 days the patient was able to practice full contact sports which is a significant decrease compared to a recent study that averaged surgical recovery time to 181 days. The recovery was supported by an MRI which demonstrated full regeneration of the previously damaged MCL. This case study demonstrates the potential stem cells have in both complementing and replacing surgical treatments for tissue repair. In addition, this case study demonstrates the efficacy of accelerating recovery of MCL tears using stem cells which inspires hope of using stem cells in similar pathologies. Therefore, more clinical trials should be conducted to further expand research on stem cell treatment in regenerative medicine.
Introduction
The Medial collateral ligament (MCL) is the most common knee injury in high school and collegiate sports, particularly those involving valgus knee loading such as American football and soccer (Peterson et al., 2000; Rothenburg et al., 2016; Swenson et al., 2013). The most common mechanism of injury of the MCL is due to valgus stress or impact applied to the lateral knee, or a combination of valgus force and external rotation of the tibia (Laprade et al., 2012; Lundblad et al., 2019; Peterson et al., 2000). MCL injuries are classified as Grade I, with minimal torn fibers with the integrity of the MCL preserved. Grade II, incomplete tears through the ligament, and Grade III, the most severe form, complete tear through the MCL (Acevedo et. al., 2021; Sanders et. al., 2005). Grade III MCL tear management is controversial, researchers have shown that both surgical and non-surgical treatments have been effective (Marchant et. al., 2011). The selected treatment for Grade III tears, either surgical or non-surgical, would depend on other factors such as the location of the tear, the presence of bony avulsion from the medial epicondyle, open medial injuries, the interposition of the distal part of the MCL under the medial meniscus and other individualized factors (Tandogan et. al., 2016). In a recent study, the median time of recovery from surgery to full contact sport was 181 days (range= 139-204 days) in Grade III MCL injuries (Acevedo et al., 2021). With hopes of speeding up recovery and increasing effectiveness, the use of biological products, such as stem cells, has raised a significant level of attention among health professionals over the past couple of years. More specifically, health professionals have become increasingly interested in the potential stem cells have in the healing process of inflammatory diseases. Stem cells are undifferentiated cells that can divide and differentiate into other types of cells. This characteristic of stem cells inspires hope that they may potentially replace damaged tissues in the human body and restore diminished or completely lost function. Stem cells can also release a broad spectrum of trophic substances (cytokines), and paracrine effects such as the secretion of growth factors and hormones involved in angiogenesis, anti-inflammatory reactions, immunomodulation, and prevention of apoptosis (Kohli et. al., 2015; Konala et. al., 2016). Mesenchymal stem cells (MSCs) release IL- 6 and 10, prostaglandin E2, Hepatocyte growth factor, nitric oxide, TGFB1, human leukocyte antigen, and extracellular vesicles; all of these factors play an important role in immunomodulation (Kohli et. al., 2015). MSCs could be either bone marrow or adipose tissue derived. Adipose-derived stromal cells (ASC) reside in the stromal vascular fraction (SVF) of adipose tissue attached around the vessels as pericytes and periadventitial cells (van Dongen et. al., 2016). Studies have shown that after well-processed techniques, adipose-derived stromal cells may augment reperfusion and angiogenesis at the site of injection (Atalay et. al., 2021).
Case Report
A 19-Year-old soccer player had a Grade III MCL tear on the right knee on 02/04/2022. The incident occurred during a soccer match when he jumped with a malalignment knee causing valgus stress during the jump. As soon as he landed, he felt intense pain and knee instability, which limited weight bearing in the right knee. He was taken to the hospital the same day and the physical exam showed inflammation and swelling at the medial joint line. A valgus stress test showed knee instability and inability to bear weight. However, an x-ray of the knee didn’t show any fracture; therefore an MCL tear was suspected, and rest with ice was recommended. He also took NSAIDs for inflammation and pain during the first week. An MRI of the right knee was done on 06/04/2022 (4 days after the injury), which showed a Grade III tearing of the distal insertion of the superficial MCL and a Grade III tearing of the deep MCL origin on the medial femoral condyle. In seek of a faster and more effective recovery, the patient decided to try a biological treatment with stem cells. Seeking treatment, the patient came to our clinic on 18/04/2022 (14 days after the injury). After an extensive physical exam, and analyzing the previous MRI (see Figure 2.4), a treatment based on adipose-derived stem cells injection followed by guided physiotherapy was suggested and scheduled for 25/04/2022 (23 days after the injury). Adipose-derived stromal cells (ASC), were isolated by mechanical dissociation through a procedure called fractionation of adipose tissue (FAT). After the injection, the patient started a progressive individualized physical therapy plan that he continued until the entire recovery period.
Materials And Methods
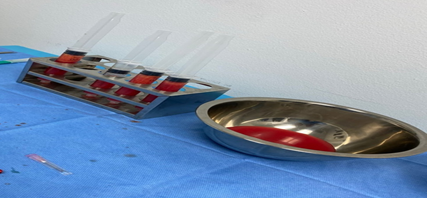
First, 500 mL of modified Klein’s solution (per 500 mL of saline, 20 mL of lidocaine, 2% epinephrine 1:200.000, and 2 mL of bicarbonate) was infused into the subcutaneous fascia to numb the area and prevent further bleeding. Adipose tissue was harvested using a lipo-harvesting cannula of 3mm x 15cm. Harvested adipose tissue was decantated in 20 mL syringes as seen in Figure 2.0, then it was centrifugated at 3.000 rpm for 2.5 minutes. After the first round of centrifugation, the oil and infiltration fluid fractions were discarded, yielding condensed lipoaspirate. In Figure 2.1, 10 mL of condensed lipoaspirate was prepared for mechanical dissociation. Two 10 mL syringes with a total volume of 10 mL of condensed lipoaspirate were connected to the fractionator (tulip) with three 1.4mm holes and 1.2mm holes. Mechanical dissociation was performed by pushing the lipoaspirate through the fractionator forwards and backward thirty times. After mechanical dissociation, the adipose tissue was centrifugated once again at 3.000 rpm for 2.5 minutes as seen in Figure 2.2. Afterward, 4 mL of the adipose tissue which contained ASCs, seen in Figure 2.3, were injected guided by ultrasound in the distal insertion of the superficial MCL and in the deep MCL origin, near the medial femoral condyle. Table 1.0 shows the number of mesenchymal stem cells that were present in the sample based on the CD markers 105 and 90 that were present in the sample after cytometry processing and that were further injected into the patient.
Figure 2.0. Harvested adipose-derived stem cells decanted in 20 mL syringes.
Figure 2.1. Condensed lipoaspirate was produced after the first round of centrifugation.
Figure 2.2. Mechanical dissociation of the lipoaspirate between two 10 mL syringes connected by a fractionator.
Figure 2.3. Injection of the adipose-derived stem cells into the distal insertion of the superficial MCL and in the deep MCL origin guided by ultrasound imaging.
Table 1.0: (Adipose Tissue sample after cytometry processing)
Post-Processing | |
| Volume | 17 ml |
| TNC (x10^6) | 195.5 x 106 |
| Sample Viability | 95.65% |
| CD105+ | 44.38 x 106 |
| CD90+ | 86.99 x 106 |
| Sterility | Negative, No Bacterial Growth |
Figure 2.4. 06/04/2022 MRI scan of the patient’s distal medial collateral ligament of the knee joint. The scan demonstrates a Grade III tear of the distal insertion of the superficial MCL and the deep MCL origin on the medial femoral condyle.
Figure 2.5.: 08/24/2022 The MRI scan demonstrates a Grade I distal MCL sprain with underlying pretibial fluid and no evidence of an MCL ligament tear.
Statistical Analysis
In this case study, a statistical analysis is not applicable. The methods and results are gathered from qualitative data as demonstrated by the MRI scans and procedure documentation.
Results And Discussion
The results of this study demonstrate the efficiency of stem cells not only in regenerating tissue but in accelerating the recovery time of Grade III MCL tears in this case study. Upon patient consultation, the patient reported returning to practice full-contact sports 100 days after receiving the adipose-derived stem cells treatment and 122 days after the MCL injury. As previously mentioned, the average time of recovery from surgical treatment in Grade III MCL tears is 181 days with a range between 139 to 204 days (Acevedo et al., 2021). Moreover, another study averages the return to play assessment to approximately 20 weeks post-operatively in Grade III MCL injuries (Logan et al., 2016). In this case study, the non-surgical treatment using adipose-derived stem cells significantly reduced the recovery time to approximately 59 days compared to the 181 means of the mentioned study. This is approximately a 32.5
Conclusion
In this study, the recovery time of a Grade III MCL tear using adipose-derived mesenchymal stem cells injection into the site of injury was compared to the recovery time of surgical treatment. The results support that the recovery time of the injury was significantly reduced in the non-surgical stem cell approach compared to surgical procedures. Using stem cells to regenerate damaged tissue and restore function proves to be an effective treatment in accelerating recovery time in this case report. This case report not only showed an accelerated recovery compared to other invasive treatments but also helped prevent a surgical intervention. Moreover, more research on the efficacy of adipose-derived MSCs in regenerative medicine should be conducted to further future applications and expand the field.
Acknowledgments
This study was not financially supported or provided with resources from any organization. The three authors of this case study solely contributed to the execution and publication of the study.
Conflict Of Interest Statement
The authors declare no potential conflict of interest with respect to the study, authorship, and/or publication of this case study.
Ethics Statement
The authors confirm that the case study follows the ethical guidelines of the journal and it has been approved by the appropriate ethical review committee. The study conformed to the US Federal Policy for the Protection of Human Subjects.
References
- Acevedo, J., Boden, A. L., Greif, D. N., Emerson, C. P., Ruiz, J. T., Jose, J., Feigenbaum, L. A., & Kaplan, L. D. (2021). Distal medial collateral ligament grade iii injuries in collegiate football players: Operative management, rehabilitation, and return to play. Journal of Athletic Training, 56(6).
View at Publisher | View at Google Scholar - Atalay, S., Coruh, A., & Deniz, K. (2014). Stromal vascular fraction improves deep partial thickness burn wound healing. Burns, 40(7).
View at Publisher | View at Google Scholar - Bagwell, M. S., Wilk, K. E., Colberg, R. E., & Dugas, J. R. (2018). THE USE OF SERIAL PLATELET RICH PLASMA INJECTIONS WITH EARLY REHABILITATION TO EXPEDITE GRADE III MEDIAL COLLATERAL LIGAMENT INJURY IN A PROFESSIONAL ATHLETE: A CASE REPORT. International Journal of Sports Physical Therapy, 13(3).
View at Publisher | View at Google Scholar - Kohli, N., Wright, K. T., Sammons, R. L., Jeys, L., Snow, M., & Johnson, W. E. B. (2015). An in vitro comparison of the incorporation, growth, and chondrogenic potential of human bone marrow versus adipose tissue mesenchymal stem cells in clinically relevant cell scaffolds used for cartilage repair. Cartilage, 6(4).
View at Publisher | View at Google Scholar - Konala, V. B. R., Mamidi, M. K., Bhonde, R., Das, A. K., Pochampally, R., & Pal, R. (2016). The current landscape of the mesenchymal stromal cell secretome: A new paradigm for cell- free regeneration. In Cytotherapy (Vol. 18, Issue 1).
View at Publisher | View at Google Scholar - Kuo, C. K., & Tuan, R. S. (2008). Mechanoactive tenogenic differentiation of human mesenchymal stem cells. Tissue Engineering Part A, 14(10), 1615-1627.
View at Publisher | View at Google Scholar - Laprade, R. F., & Wijdicks, C. A. (2012). The management of injuries to the medial side of the knee. journal of orthopaedic & sports physical therapy, 42(3), 221-233.
View at Publisher | View at Google Scholar - Logan, C. A., O’Brien, L. T., & LaPrade, R. F. (2016). POST OPERATIVE REHABILITATION OF GRADE III MEDIAL COLLATERAL LIGAMENT INJURIES: EVIDENCE BASED REHABILITATION AND RETURN TO PLAY. International Journal of Sports Physical Therapy, 11(7).
View at Publisher | View at Google Scholar - Logan, C. A., O'Brien, L. T., & LaPrade, R. F. (2016). Post operative rehabilitation of grade III medial collateral ligament injuries: evidence based rehabilitation and return to play. International journal of sports physical therapy, 11(7), 1177.
View at Publisher | View at Google Scholar - Marchant, M. H., Tibor, L. M., Sekiya, J. K., Hardaker, W. T., Garrett, W. E., & Taylor, D. C. (2011). Management of medial-sided knee injuries, part 1: Medial collateral ligament. American Journal of Sports Medicine, 39(5).
View at Publisher | View at Google Scholar - Peterson, L., Junge, A., Chomiak, J., Graf- Baumann, T., & Dvorak, J. (2000). Incidence of football injuries and complaints in different age groups and skill-level groups. American Journal of Sports Medicine, 28(5 SUPPL.).
View at Publisher | View at Google Scholar - Rothenberg, P., Grau, L., Kaplan, L., & Baraga, M. G. (2016). Knee injuries in American football: an epidemiological review. Am J Orthop, 45(6), 368-373.
View at Publisher | View at Google Scholar - Sanders, T. G., & Miller, M. D. (2005). A systematic approach to magnetic resonance imaging interpretation of sports medicine injuries of the knee. The American journal of sports medicine, 33(1), 131-148.
View at Publisher | View at Google Scholar - Swenson, D. M., Collins, C. L., Best, T. M., Flanigan, D. C., Fields, S. K., & Comstock, R. D. (2013). Epidemiology of knee injuries among US high school athletes, 2005/06–2010/11. Medicine and science in sports and exercise, 45(3), 462.
View at Publisher | View at Google Scholar - Tandogan, N. R., & Kayaalp, A. (2016). Surgical treatment of medial knee ligament injuries: Current indications and techniques. EFORT Open Reviews, 1(2), 27-33.
View at Publisher | View at Google Scholar - Van Dongen, J. A., Stevens, H. P., Parvizi, M., van der Lei, B., & Harmsen, M. C. (2016). The fractionation of adipose tissue procedure to obtain stromal vascular fractions for regenerative purposes. Wound repair and regeneration, 24(6), 994-1003.
View at Publisher | View at Google Scholar