Research Article | DOI: https://doi.org/10.58489/2836-8649/008
A Retrospective Clinical Evaluation of Esthetic Restorations: Class III, IV, And V
1DDS; MSc, Department of Conservative Dentistry, Federal University of Rio Grande do Sul, RS, Brazil.
2DDS; MSc; PhD, Department of Conservative Dentistry, Federal University of Rio Grande do Sul, RS, Brazil.
*Corresponding Author: Rodrigo Monteiro Vieira
Citation: Rodrigo Monteiro Vieira, Maria Carolina Guilherme Erhardt, Fabio Herrmann Coelho-de-Souza. (2024). A Retrospective Clinical Evaluation of Esthetic Restorations: Class III, IV, And V. Journal of Dental and Oral Care. 3(1); DOI: 10.58489/2836-8649/008
Copyright: © 2024 Rodrigo Monteiro Vieira, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 10 February 2024 | Accepted: 01 March 2024 | Published: 02 March 2024
Keywords: Composite Resins. Permanent Dental Restoration. Retrospective Studies.
Abstract
This study aimed to evaluate direct composite restorations Class III, IV and V through the USPHS and FDI criteria. Eighty-seven patients were selected through a search of the patients’ records present in the School of Dentistry. Restorations performed between 2000 to 2013 which a minimum of six months in service were selected. Adult patients of both sexes were included, who received composite restorations with total-etch adhesive system; on vital and non-vital teeth. Clinical evaluation was performed by USPHS and FDI criteria, by one calibrated examiner. The survival of the restorations was analyzed using the Kaplan-Meier and log-rank test to compare groups, and multivariate Cox regression and hazard ratio were employed to identify factors associated with the failure of the restorations. 272 restorations were evaluated with a time interval in service from 8 months to 13 years (mean 4.8 years). 120 class III restorations were evaluated with 15 failures (12.5%), with an annual failure rate of 2.74%. For class IV, 80 restorations were evaluated, with 38 failures (47.5%), with an annual failure rate of 12.6%. And for class V, 72 restorations were analyzed, with the presence of failures in 27 of them (37.5%), with annual failure rate of 9.3%. The most common reason for failure was fracture and loss of retention, occurring in 73 cases in total. Non-vital teeth showed 50% of failure, with an annual failure rate of 13.4%; while the vital teeth showed 28.1% of failure, with an annual failure rate of 6.6%. It was concluded that composite restorations showed a satisfactory performance over time, with a survival rate of 70.6% in a mean time of 4.8 years. Class III showed better clinical performance than class V and IV. Non-vital teeth restorations had 2.37 times the risk of failures than vital teeth. Both criteria (USPHS and FDI) were effective in the clinical evaluation process.
Introduction
The advance of the adhesive systems and composite resins in the last decades provided important changes in the restorative treatments practiced in dentistry (Geitel et al., 2004). Before that, anterior and posterior teeth needed retentive preparations often wearing expressively the dental remaining in order to increase the frictional retention and longevity of restorations. Because of their development and fast improvement, the composites are used in most of the restorations in anterior teeth nowadays, being considered the material of choice in direct aesthetic and functional rehabilitations (Ermis et al., 2010; Baldissera et al., 2013). Due to its advantages such as the possibility to be used in conservative preparations, preserving dental structure, lower cost, aesthetics, less time consuming and the repair capacity, the composites are the first choice for esthetic restorations when compared to indirect materials (Heintze, Rousson, Hickel, 2015; Demarco et al, 2015).
Although the composites are very well accepted in the scientific and academic environment, there are some limitations of the material itself that should not be ignored. The polymerization shrinkage is one of those features that can compromise the clinical performance of the restorations. The effects of shrinkage can generate marginal staining (leakage), marginal gap, post-operative sensitivity and cracks in the enamel (Carvalho et al., 1996). The sensitive technique is another disadvantage that has to be confronted when working with composites, because the material is not compatible with humidity (Van Meerbeek et al., 2003). The final result of the direct restorations also depends on the dentist's ability to reproduce anatomical details and optical characteristics, especially when it comes from anterior teeth, mimetizing the natural teeth as best as possible (Poyser et al., 2007).
There are currently on the market several types of composites. The differences among composites’ brands are related to the composition, particle size, mechanical properties and optical characteristics. The microhybrid, nanohybrid and nanofilled composites are considered as universal indication because they are used for both anterior and posterior teeth. These composites have good optical and mechanical characteristics, combined with the size and amount of the inorganic particles in its composition (Da Rosa Rodolpho et al., 2011; Coelho-de-Souza et al, 2015). On the other hand, microfilled composites are indicated in situations where resistance is not required, and should be used in the labial surface, due to its excellent optical characteristics and polishing (Heintze, Rousson, Hickel, 2015; Van Djiken, Pallesen, 2010; Coelho-de-Souza et al, 2015).
The literature shows a lack of long-term in vivo studies evaluating composite restorations in anterior teeth. For those analyses, clinical trials and practice-based research are the best options, because they generate more reliable clinical evidence and consistent results, when compared to laboratory studies, which are more distant from the clinical reality. In this context, retrospective studies seems to be an alternative methodology to evaluate many restorations in a short period of time, revealing the quality of the procedures in a real life analysis (Van de Sande et al, 2013, Baldissera et al, 2013, Demarco et al, 2015, Coelho-de-Souza et al, 2015).
Although the typical types of aesthetic restorations in anterior teeth (class III, IV and V) are procedures very practiced nowadays, these are not sufficiently discussed in the literature, having few clinical studies and short follow-up time (Gresnigt, Kalk, Ozcan, 2012; Reusens, D'Hoore, Vreven, 1999). Therefore, the aim of this retrospective study is to provide a clinical evaluation of esthetic composite restorations, showing the clinical reality of the restorations in daily practice.
Materials And Methods
Study design and ethical considerations
The research protocol (21736) of this study had the approval of the Ethics Committee, Federal University of Rio Grande do Sul (UFRGS, Porto Alegre, Brazil). This study is a retrospective and blind clinical evaluation of direct esthetic composite restorations Class III, IV and V (proximal and cervical of anterior teeth and premolars). All patients signed an informed consent before joining the study.
Sample size
The sample size necessary to the study was calculated based on a 90% confidence interval, a presumed error of 10%, and a percentage of secondary caries outcome of 22.4% (Da Rosa Rodolpho et al., 2006). The minimum value of n was 47 restorations.
Selection of patients
Inclusion and exclusion criteria were considered for selection of the study population (Coelho-de-Souza et al, 2015). Patients’ records were assessed in the Federal University of Rio Grande do Sul. Adult patients who received treatment with direct composite restorations class III, IV or V in anterior teeth or gingival third of premolars with a minimum of 06 months in service, in vital and non-vital teeth were included in this study. Patients with poor oral hygiene or with special needs were excluded of this survey. Restorations were considered for evaluation when placed between 2000 to 2013, performed by undergraduate students.
Restorative procedures
The dentin-bonding agent used in all composite restorations was a total-etch 3-step adhesive system. Restorations were built with one of the evaluated composites described in Table 1. Composite restorations were built under rubber dam, with an incremental technique and were light-cured using an LED polymerization unit. The restorations were finished and polished in the same session using fine diamond burs, abrasive rubber cups and abrasive discs.
Evaluation procedures
A total of 110 patients were selected for the evaluation process; however, 87 agreed to participate in the survey, and they were included in the study (35 men and 52 women), with 272 restorations. From the files, the type of the composite, the tooth vitatily (vital or non-vital) date of placement, date of failure and reason for failure were collected.
Patients were contacted by phone to come in one of the clinics of the School of Dentistry at UFRGS on predetermined date for conducting the evaluations. After signed the informed consent, the patient was clinically evaluated by one examiner trained and calibrated by the Cohen’s Kappa coefficient and blind to the study aims, regarding the composite brand and time in service of the restoration. The Cohen’s Kappa calculation was made by repeating the evaluation of some restorations twice in different sessions, randomly selected.
The visual evaluation was assisted by explorer probe, dental mirror and light reflector, and performed after prophylaxis of teeth with a rubber cup and prophylaxis paste. Those patients who presented treatment needs found in clinical evaluation were referred to the clinics at school graduation. The evaluation criteria used in the study were the modified USPHS and FDI, including the aesthetic, functional and biological properties (Ryge, 1980; Hickel et al, 2007). Scores C (USPHS), and 4 or 5 (FDI) were considered as failure (clinically unacceptable). When restorations had failed before the examination, date and reason for failure were recorded from the patients’ files. Also, for bruxism evaluation, patients were asked about the habit of grinding or clenching during the day or night, pain reports, muscle or joint fatigue and if had been diagnosed with a functional disorder.
Table 1. Characteristics and properties of the evaluated composites*:
| COMPOSITE | MANUFACTURER | Inorganic filler classification | E - MODULUS (GPA) | INORGANIC Filler percentage | Mean PARTICLE SIZE | CLINICAL INDICATION | N restorations |
| Charisma | Heraeus Kulzer | Microhybrid | 14.06 | 59.4 vl | 0.7 µm | Anterior and posterior teeth | 80 |
Z350 XT/ Supreme | 3M/ESPE | Nanofill | 13.3 | 63.3vl | 20-75nm | Anterior and posterior teeth | 90 |
| Opallis | FGM | Nanohybrid | 9.1 | 58 vl | 0.5 µm | Anterior and posterior teeth | 25 |
| Esthet-X | Dentsply | Nanohybrid | 12.3 | 77 wt | 0.6-0.8 µm | Anterior and posterior teeth | 53 |
| Fill magic | Vigodent | Microhybrid | 3.9 | 57 vl | 0.5 µm | Anterior and posterior teeth | 13 |
| Durafill VS | Heraeus Kulzer | Microfill | 6.15 | 37.5 vl | 0.04 µm | Anterior teeth | 11 |
*(Garcia et Al., 2006; Bicalho et Al., 2014; Baldissera et Al., 2013; Loomans et Al., 2008; Willems et Al., 1992; Kim; Ong; Okuno, 2002; Nagem Filho et Al., 2007; Barkmeier et Al., 2015).
Data analysis
The data obtained in the clinical evaluation were tabulated and subjected to statistical analysis. The survival of restorations over time was analyzed using the Kaplan-Meier method and log-rank test to compare the groups. Multivariate Cox regression with shared frailty and hazard ratio were employed to identify factors associated with the failure of the restorations. The significance level for all analyzes was 5%. The annual failure rates for all types of restorations were calculated. Multiple observations were done in some patients.
Results
The distribution of restorations according to the independent variables is shown in Table 2. In total, 272 restorations were evaluated in 87 adult patients (mean age 52 years old), with an overall survival rate of 70.6% (80 failures; annual failure rate – AFR 6.9%). The follow-up time varied from 8 months up to 13 years with a mean observation time of 4.8 years.
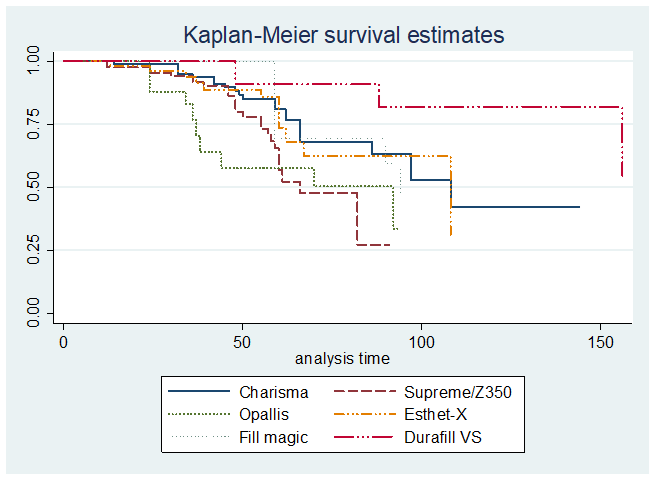
The 6 composites’ brands of the 272 evaluated restorations and their respective sampling numbers were: Z350 XT (90), Charisma (80), Esthet-X (56), Opallis (25), Fillmagic (13) and Durafill VS (11). Their characteristics and properties are shown in Table 1.
In Tables 3 and 4, the qualitative evaluation using USPHS and FDI criteria of the restorations are shown.
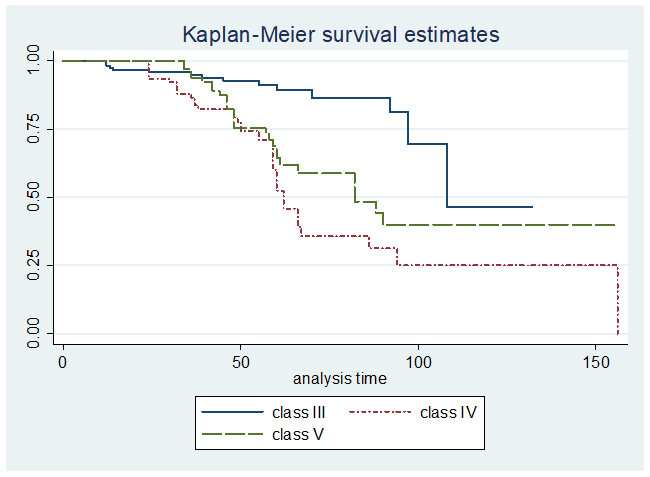
In Figures 1, 2 and 3, the Kaplan-Meier survival curves show the clinical behavior for composite restorations in different class types, brands and tooth vitality, with significant differences (log-rank: p<0 p=0.0032 p=0.0249,>
In Table 5, the adjusted Cox Regression analyses showed that restorations performed in non-vital teeth had a risk of failure of 2.37 times higher than those placed in vital teeth. Also, there is association among the composite brands and the class type with the failure outcome.
For class III restorations, there were 120 restorations evaluated with 15 failures (12.5%) and the AFR was 2.74%. For class IV restorations, there were 80 restorations evaluated with 38 failures (47.5%) and the AFR was 12.6%. For class V restorations, there were 72 restorations evaluated with 27 failures (37.5%) and the AFR was 9.3%. The most common reason for failure was fracture and loss of retention for classes III, IV, and V, occurring in 73 cases. Non-vital teeth had 50% of failure in a mean time of 4.8 years with the annual failure rate (AFR) of 13.4%; while vital teeth had 28.1% of failure and AFR of 6.6%.
Table 2: Distribution of restorations according to the independent variables.
Independent variables | N | % |
Sex Male Female Total |
35 52 87 | 40,2% 59,8% 100% |
Teeth Central incisor Lateral incisor Canine Premolar Total | 99 84 59 30 272 | 36,4% 30,9% 21,7% 11% 100% |
Follow-up (years) 0.5 - 2 2 - 4 4 - 6 6 – 8 8 – 10 10-13 Total | 27 77 115 37 6 10 272 | 9,9% 28,3% 42,3% 13,6% 2,2% 3,7% 100% |
Composite resin Charisma Z350 XT Opallis Esthet-X HD Fill magic Durafill VS Total |
80 90 25 53 13 11 272 |
29,4% 33,1% 9,2% 19,5% 4,8% 4% 100% |
Bruxism Yes No Total | 55 217 272 | 20,2% 79,8% 100% |
Vitality Vital Not vital Total | 256 16 272 | 94,1% 5,9% 100% |
Class Class III Class IV Class V Total |
120 80 72 272 |
44,1% 29,4% 26,5% 100% |
Table 3: Clinical evaluation of composite restorations, according to the USPHS criteria (Ryge, 1980):
|
| Class III | Class IV | Class V | |||
|
| Scores* n (A/B/C) | Restorations clinically acceptable | Escores n (A/B/C) | Restorations clinically acceptable | Scores n (A/B/C) | Restorations clinically acceptable |
Aesthetics properties | Anatomic form Luster and roughness | 109 (67/42/0) 109 (45/64/0) | 100% 100% | 57 (17/37/3) 57 (17/39/1) | 94,7% 98,2% | 46 (23/23/0) 46 (24/22/0) | 100% 100% |
| Marginal staining | 109 (18/91/0) | 100% | 57 (10/45/2) | 96,4% | 46 (14/32/0) | 100% |
| Color match | 109 (74/35/0) | 100% | 57 (38/19/0) | 100% | 46 (31/15/0) | 100% |
Functional properties | Fracture and retention | 120 (109/0/11) | 90,8% | 79 (43/0/36) | 54,4% | 72 (46/0/26) | 63,8% |
| Marginal integrity | 109 (33/76/0) | 100% | 57 (8/49/0) | 100% | 46 (12/34/0) | 100% |
Biological properties | Secondary caries | 109 (105/0/4) | 96,3% | 58 (57/0/1) | 98,2% | 47 (46/0/1) | 97,8% |
| Postoperative sensitivity | 109 (109/0/0) | 100% | 57 (57/0/0) | 100% | 46 (46/0/0) | 100% |
*For each evaluation criterion a score from A to C is given: A and B when the restoration is clinically acceptable, while C designate failure. Kappa 0.87.
Table 4: Clinical evaluation of composite restorations, according to the FDI criteria (Hickel et al, 2007):
|
| Class III | Class IV | Class V | |||
|
| Scores* n (1/2/3/4/5) | Restorations Clinically Acceptable | Scores n (1/2/3/4/5) | Restorations Clinically Acceptable | Scores n (1/2/3/4/5) | Restorations Clinically Acceptable |
Aesthetics properties | Surface luster | 109 (39/63/7/0/0) | 100% | 57 (13/43/1/0/0) | 100% | 46 (21/20/5/0/0) | 100% |
|
| 109 (42/56/11/0/0) | 100% | 57 (25/29/3/0/0) | 100% | 46 (25/18/3/0/0) | 100% |
|
| 109 (11/57/41/0/0) | 100% | 57 (10/30/15/2/0) | 96,4% | 46 (12/19/15/0/0) | 100% |
|
| 109 (66/36/7/0/0) | 100% | 57 (35/21/1/0/0) | 100% | 46 (28/15/3/0/0) | 100% |
|
| 109 (68/38/3/0/0) | 100% | 57 (18/23/13/3/0) | 94,7% | 46 (23/18/5/0/0) | 100% |
Functional properties | Fracture and retention | 120 (102/4/3/0/11) | 90,8% | 79 (33/4/6/14/22) | 54,4% | 72 (39/2/5/0/26) | 63,8% |
| Marginal adaptation | 109 (23/81/5/0/0) | 100% | 57 (7/43/7/0/0) | 100% | 46 (9/30/7/0/0) | 100% |
| Patient’s view | 109 (68/26/15/0/0) | 100% | 58 (28/9/16/2/3) | 91,3% | 46 (31/10/5/0/0) | 100% |
Biological properties | Recurrence of caries, erosion and abfraction | 109 (101/1/3/4) | 93,5% | 58 (53/0/4/0/1) | 98,2% | 47 (38/4/3/1/1) | 95,7% |
| Postoperative sensitivity | 109 (108/1/0/0/0) | 100% | 57 (57/0/0/0/0) | 100% | 46 (46/0/0/0/0) | 100% |
*For each evaluation criterion a score from 1 to 5 is given: 1-3 when the restoration is clinically acceptable, while 4 and 5 designate failure. Kappa 0.87.
Fig 1: Kaplan-Meier survival curves for composite restorations in different class type cavities (log-rank: p<0>
Fig 2: Kaplan-Meier survival curves for composite restorations with different brands (log-rank: p=0.0032) (time in months).
Fig 3: Kaplan-Meier survival curves for composite restorations in vital and non-vital teeth (log-rank: p=0.0249) (time in months).
Table 5: Cox regression analysis with adjusted Hazard Ratio (HR) for independent variables and failures of composite restorations.
Independent variables | HR | 95% conf. interval | p-value |
Sex | 0.84 | 0.53 – 1.34 | 0.475 |
Tooth type | 0.85 | 0.66 – 1.07 | 0.169 |
Material | 0.83 | 0.75 – 0.94 | 0.002 |
Tooth vitality | 2.37 | 1.10 – 5.11 | 0.027 |
Bruxism | 1.44 | 0.84 – 2.47 | 0.180 |
Class type | 1.95 | 1.40 – 2.70 | <0> |
Discussion
This retrospective study evaluated the clinical performance of composite restorations class III, IV and V in anterior teeth and premolars using the USPHS and FDI criteria. Even though the randomized clinical trials are considered the gold standard to evaluate the longevity of restorations, with a better control of variables, the retrospective studies have some advantages (Baldissera et al., 2013; Kim, Namgung, Cho, 2013). This kind of study design needs a short period of time and low cost to be conducting. Retrospective studies can be an interesting alternative for a long-term performance evaluation, showing the reality of the restorations in a daily practice (real life) (Manhart et al., 2004, Baldissera et al, 2013, Coelho-de-Souza et al, 2015, Van de Sande et al, 2013).
In the current study, we could observe a variability of the results of the clinical performance for different restoration types, with an annual failure rate of 2.74%, 12.6% and 9.3% for classes III, IV and V, respectively. These findings are comparable to results obtained in university environment studies (Moura et al., 2011; Lynch et al., 2010), which students perform the restorative procedures, with a large number of operators and a population with a low socioeconomic status. Other studies carried out in private clinics could have slightly different outcomes. In these cases, the care is performed by a dentist, assisting patients with better socioeconomic conditions, greater self-care and access to information, including preventive maintenance appointments (Baldissera et al., 2013). Correa et al. (2013) showed that the socioeconomic status of the individual can affect the durability of the restorations.
Some previous studies reported that the cavity type and its location can influence the longevity of restorations (Da Rosa Rodolpho et al., 2006; Moura et al., 2011; Manhart et al., 2004; Opdam et al., 2007; Mjor et al., 2002; Baldissera et al., 2013; Heintze; Rousson; Hickel, 2015). In our study, the results were similar, significant differences among classes of restorations (III, IV and V) were found. This is due to cavities with different etiologies, locations and behaviors (Demarco et al, 2015). Further, the major cause of failure for class III restorations was fractures and retention, followed by secondary caries, unlike exposed in early studies, which suggest secondary caries as the main reason for failure. Van Noort and Davis (1993), in a prospective study, appointed that the major cause of failure for class III was secondary caries and surface staining, although the type of composite used was chemically activated. Deligeorgi et al. (2000) reported 35% of failure rate for secondary caries being the main cause of operative interventions in class III. Demerci et al. (2006), in a longitudinal clinical study, evaluated proximal anterior teeth restorations after 5 years, and reported that the higher failure rate was also by secondary caries (8%). However, in recent studies, such as Baldissera et al. (2013) and Coelho-de-Souza et al (2015), fractures and loss of retention were the main reason for failures, either in a private clinic or university studies, respectively. In the present study, although the people who received the restorations were from lower socioeconomic status, and therefore with higher risk of caries (Correa et al., 2010; Correa et al., 2013), they were mostly adult and elder people, being in an age group with lower risk of caries (Correa et al, 2010; Correa et al, 2013), compared with adolescents and children groups. In addition, it is important to highlight the evolution in public health regarding the access to information and the use of fluoride in the Brazilian poorest areas (Baldani et al., 2011; Van De Sande et al., 2013).
Previous studies suggested greater clinical longevity for class III restorations when compared to class IV, because of the cavity position in a low-stress area and it is surrounded by enamel (Baldissera et al., 2013; Smales, 1991). The main reason for failures found in class IV restorations was fracture and retention (Moura et al., 2011; Baldissera et al., 2013; Van Djiken, Pallensen, 2010; Smales, 1991; Heintze, Rousson, Hickel, 2015). This type of restoration is adhered in a fewer number of walls and its extension compromises the incisal edge. In this current study, class III restorations had a survival rate of 87.5% with an annual failure rate of 2.74% at an average of 4.8 years, while the class IV showed a different performance, resulting in 52.5% survival rate with an annual failure rate of 12.6%. Other studies have found similar results for class IV restorations. Browning and Dennison (1996) found a failure rate of 36% at 3 years of follow-up and 50% at 5 years for class IV. Burke et al. (1999) showed a mean longevity time of 3.9 years for class IV. On the other hand, Baldissera et al (2013) demonstrated a lower failure rate (annual failure rate between 0.5% and 1.8%) for the same kind of restorations, which can be explained by the number and quality of the operators (one specialist/postgraduate), besides the high socioeconomic level of patients in a private clinic. In contrast, our study was carried out in a public university environment, the restorations were performed by undergraduate students and several operators, and the patients had lower socioeconomic status, as seen in Coelho-de-Souza et al (2015).
Cervical restorations (class V) are the most often studied in the literature among anterior restorations nowadays (Peumans et al., 2012; Namgung et al., 2012; Qin et al., 2013). Because of its expulsive cavity characteristics, combined with a large area of dentin and a little amount or no cervical enamel are considered a major challenge for the adhesion. In general, the composite has been the material of choice for cervical lesions due to aesthetics, good polishing, bond strength and versatility (Folwaczny et al., 2001). However, as already mentioned, restore these lesions with composite resin faces a number of technical difficulties that may affect the clinical outcomes. Difficulties in field isolation, in adhesion with the dentin margin and the expulsive aspect of the cavity make the procedure considered as a highly sensitive technique (Chang et al., 2010; Cho et al., 2002). In our study, the highest failure rate was fractures and loss of retention, occurring in 26% of the restorations. Lower failure rates by retention are identified after 12 years of evaluation by Wilder et al. (2009), 11%, and after 13 years by Boghosian, Drummond and Lautenschlager (2007), 3%. However, in Van Dijken and Pallensen (2008), after 13 years, a 40% of failure rate was identified.
We could observe a significant difference in the failure rate between vital and non-vital teeth, as seen in Coelho-de-Souza et al (2015) for composite veneers. According to the Cox regression analysis, non-vital teeth had 2.37 times the risk of failure than vital teeth. This can be attributed to some factors, such as: endodontically treated teeth usually have greater loss of tooth structure due to the access to the endodontic treatment, extension of caries lesions and previous restorations. Mondelli et al. (1980), in an in vitro study, evaluated the fracture resistance of teeth with different sizes of cavity preparations, and concluded that the greater the loss of tooth structure, the lower the resistance to fracture; as well as Coelho-de-Souza et al., (2008). Previous clinical studies have shown that the bigger restorations (more compromised surfaces) have a higher risk of failures (Da Rosa Rodolplho et al., 2006; Da Rosa Rodolplho et al., 2011; Baldissera et al., 2013). Although the sample of non-vital teeth found in this current study was small, it was possible to realize a percentage of failure of the group of non-vital teeth, showing a 50% of failure in a mean period of 4.8 years. It is suggested that future studies should be conducted with larger samples in order to do a more accurate analysis comparing restorations in vital and non-vital teeth (Coelho-de-Souza et al, 2015).
According to statistical analysis, a significant difference between the materials’ brands used was noticed. However, a wide variety of composite types were evaluated (Charisma, Durafill VS, Opallis, Z350XT, Fillmagic e Esthet-X) with different sample numbers (ranging from 11 to 90). Thus, the comparison among them does not become reliable. In the literature, there are few studies comparing composite characteristics, brands and different particle sizes (Van Djiken; Pallesen, 2010; Karaman et al., 2012). Baldissera et al. (2013), in a retrospective study, made a comparison of two composite brands in anterior teeth: Herculite XR and Charisma. Herculite XR showed better performance according the FDI criteria. Another important point to highlight in this current study is the use of the same dentin-bonding agent for all restorations evaluated: a 3-step total-etch adhesive system. This dentin-bonding agent is considered the "gold standard" supported by several studies (Dantas et al., 2008; Ahmed et al., 2013).
Several researchers still prefer to use the USPHS criteria for clinical evaluation, due to its simplicity and longtime of using (Ryge, 1980; Millar, Robinson, Inglis, 1997; Geitel et al., 2004; Da Rosa Rodolpho et al., 2006; Qin et al., 2013). However, more sensitive and completed criteria would be interesting to improve the quality of the clinical evaluation (Hickel et al., 2007). The FDI criteria (Hickel et al, 2007, Hickel et al, 2010) has been used in some clinical studies as alternative and more detailed method of evaluation since 2007 (Baldissera et al., 2013, Coelho-de-Souza et al, 2015). Some examples of the changes in FDI criteria include the staining accessing, divided in marginal and superficial, due to the fact that they are from different causes and do not appear simultaneously, as it can be noticed in this study. The 5 evaluation scores of FDI criteria, unlike the USPHS, can make a more detailed identification of the failures (scores 4 and 5). The failure is divided in repairable (score 4) or replacement indicated (score 5). Another difference between the two criteria is the evaluation of non-carious lesions, an important addition proposed by the FDI. It is noticed in this study, in the criterion “recurrence of caries, erosion, abrasion and abfraction” (FDI), there was 6.5% of failure, whereas the parallel criterion in USPHS, “secondary caries”, presented 3.7% of failure. The "patient's opinion" criterion suggested by the FDI is also an interesting addition, considering the esthetic standards of the patients, especially for anterior restoration presented in this study. Nevertheless, although the differences between the USPHS and FDI, both methods can be used for clinical evaluation, regarding the qualitative analysis.
Considering the findings of this current study, it is important to point out the differences among the performance and failure rate of the class III, IV and V restorations, regarding the risk of their location and characteristics associated with the tooth. Comparing the three types of restoration, class III has the lowest risk of failure (2.74% annual failure rate), followed by class V and class IV (annual failure rate of 9.3% and 12.6%, respectively). Furthermore, it is interesting to emphasize the higher failure rate of restorations placed in non-vital teeth, when compared to vital teeth. Other prospective long-term studies must be conducted to confirm these findings. Different types of adhesive systems and composite brands are also interesting alternatives for future research in this subject, especially when dealing with class IV restorations.
Conclusion
It is possible to conclude that composite restorations demonstrated a satisfactory clinical performance over time, with a survival rate of 70.6% in general, in a mean time of 4.8 years. Class III restorations showed better clinical performance with lower annual failure rate than class V and class IV. The restorations placed in non-vital teeth had 2.37 times the risk of failures than restorations in vital teeth. Fracture and loss of retention were the main reasons for failure for all types of restoration. Both criteria (USPHS and FDI) were effective in the clinical evaluation process.
References
- Ahmed, W., El-Badrawy, W., Kulkarni, G., Prakki, A., & El-Mowafy, O. (2013). Gingival microleakage of class V composite restorations with fiber inserts. The Journal of Contemporary Dental Practice, 14(4), 622.
View at Publisher | View at Google Scholar - Baldani, M. H., & Antunes, J. L. F. (2011). Inequalities in access and utilization of dental services: a cross-sectional study in an area covered by the Family Health Strategy. Cadernos de Saúde Pública, 27(suppl 2), s272-s283.
View at Publisher | View at Google Scholar - Baldissera, R. A., Corrêa, M. B., Schuch, H. S., Collares, K., Nascimento, G. G., Jardim, P. S., ... & Demarco, F. F. (2013). Are there universal restorative composites for anterior and posterior teeth?. Journal of dentistry, 41(11), 1027-1035.
View at Publisher | View at Google Scholar - Barkmeier, W. W., Takamizawa, T., Erickson, R. L., Tsujimoto, A., Latta, M., & Miyazaki, M. (2015). Localized and generalized simulated wear of resin composites. Operative dentistry, 40(3), 322-335.
View at Publisher | View at Google Scholar - Bicalho, A. A., Pereira, R. D., Zanatta, R. F., Franco, S. D., Tantbirojn, D., Versluis, A., & Soares, C. J. (2014). Incremental filling technique and composite material—Part I: Cuspal deformation, bond strength, and physical properties. Operative dentistry, 39(2), e71-e82.
View at Publisher | View at Google Scholar - BOGHOSIAN, A. A.; DRUMMOND, J. L.; LAUTENSCHLAGER, E. Clinical evaluation of a dentin adhesive system: 13-year results. J. Dent. Res., 86, special issue A, 2007.
View at Publisher | View at Google Scholar - Browning, W. D., & Dennison, J. B. (1996). A survey of failure modes in composite resin restorations. Operative dentistry, 21, 160-166.
View at Publisher | View at Google Scholar - Burke, F. J., Cheung, S. W., Möhr, I. A., & Wilson, N. H. (1999). Restoration longevity and analysis of reasons for the placement and replacement of restorations provided by vocational dental practitioners and their trainers in the United Kingdom. Quintessence International, 30(4).
View at Publisher | View at Google Scholar - Carvalho, R. M. D., Pereira, J. C., Yoshiyama, M., & Pashley, D. H. (1996). A review of polymerization contraction: the influence of stress development versus stress relief. Operative dentistry, 21(1), 17-24.
View at Publisher | View at Google Scholar - Chang, S. W., Cho, B. H., Lim, R. Y., Kyung, S. H., Park, D. S., Oh, T. S., & Yoo, H. M. (2010). Effects of blood contamination on microtensile bond strength to dentin of three self-etch adhesives. Operative dentistry, 35(3), 330-336.
View at Publisher | View at Google Scholar - Cho, B. H., Dickens, S. H., Bae, J. H., Chang, C. G., Son, H. H., & Um, C. M. (2002). Effect of interfacial bond quality on the direction of polymerization shrinkage flow in resin composite restorations. Operative Dentistry, 27(3), 297-304.
View at Publisher | View at Google Scholar - Coelho-De-Souza, F. H., Camacho, G. B., Demarco, F. F., & Powers, J. M. (2008). Fracture resistance and gap formation of MOD restorations: influence of restorative technique, bevel preparation and water storage. Operative dentistry, 33(1), 37-43.
View at Publisher | View at Google Scholar - Coelho-de-Souza, F. H., Gonçalves, D. S., Sales, M. P., Erhardt, M. C. G., Corrêa, M. B., Opdam, N. J., & Demarco, F. F. (2015). Direct anterior composite veneers in vital and non-vital teeth: a retrospective clinical evaluation. Journal of Dentistry, 43(11), 1330-1336.
View at Publisher | View at Google Scholar - Correa, M. B., Peres, M. A., Peres, K. G., Horta, B. L., Gigante, D. P., & Demarco, F. F. (2010). Life-course determinants of need for dental prostheses at age 24. Journal of dental research, 89(7), 733-738.
View at Publisher | View at Google Scholar - Correa, M. B., Peres, M. A., Peres, K. G., Horta, B. L., Barros, A. J., & Demarco, F. F. (2013). Do socioeconomic determinants affect the quality of posterior dental restorations? A multilevel approach. Journal of dentistry, 41(11), 960-967.
View at Publisher | View at Google Scholar - Dantas, D. C. R. E., Ribeiro, A. I. A. M., Lima, L. H. M. D. A., Lima, M. G. D., Guênes, G. M. T., Braz, A. K. S., & Braz, R. (2008). Influence of water storage time on the bond strength of etch-and-rinse and self-etching adhesive systems. Brazilian dental journal, 19, 219-223.
View at Publisher | View at Google Scholar - da Rosa Rodolpho, P. A., Cenci, M. S., Donassollo, T. A., Loguércio, A. D., & Demarco, F. F. (2006). A clinical evaluation of posterior composite restorations: 17-year findings. Journal of dentistry, 34(7), 427-435.
View at Publisher | View at Google Scholar - Rodolpho, P. A. D. R., Donassollo, T. A., Cenci, M. S., Loguércio, A. D., Moraes, R. R., Bronkhorst, E. M., ... & Demarco, F. F. (2011). 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dental materials, 27(10), 955-963.
View at Publisher | View at Google Scholar - Deligeorgi, V., Wilson, N. H. F., Fouzas, D., Kouklaki, E., Burke, F. J. T., & Mjör, I. A. (2000). Reasons for placement and replacement of restorations in student clinics in Manchester and Athens. European Journal of Dental Education, 4(4), 153-159.
View at Publisher | View at Google Scholar - Demarco, F. F., Collares, K., Coelho-de-Souza, F. H., Correa, M. B., Cenci, M. S., Moraes, R. R., & Opdam, N. J. (2015). Anterior composite restorations: A systematic review on long-term survival and reasons for failure. Dental materials, 31(10), 1214-1224.
View at Publisher | View at Google Scholar - Demirci M, Ersev H, Sancakli HS, Topçubaşi M. Clinical evaluation of a polyacid-modified resin composite (Dyract) in Class III cavities: 5-year results. Am J Dent. 2006 Oct;19(5):293-6. PMID: 17073207.
View at Publisher | View at Google Scholar - Ermis, R. B., Temel, U. B., Celik, E. U., & Kam, O. (2010). Clinical performance of a two-step self-etch adhesive with additional enamel etching in Class III cavities. Operative Dentistry, 35(2), 147-155.
View at Publisher | View at Google Scholar - Folwaczny, M., Mehl, A., Kunzelmann, K. H., & Hickel, R. (2001). Clinical performance of a resin-modified glass-ionomer and a compomer in restoring non-carious cervical lesions. 5-year results. American Journal of Dentistry, 14(3), 153-156.
View at Publisher | View at Google Scholar - Hervás García, A., Lozano, M., Cabanes Vila, J., Barjau Escribano, A., & Fos Galve, P. (2006). Composite resins: a review of the materials and clinical indications.
View at Publisher | View at Google Scholar - Geitel, B., Kwiatkowski, R., Zimmer, S., Barthel, C. R., Roulet, J. F., & Jahn, K. R. (2004). Clinically controlled study on the quality of Class III, IV and V composite restorations after two years. Journal of Adhesive Dentistry, 6(3).
View at Publisher | View at Google Scholar - Gresnigt, M. M., Kalk, W., & Özcan, M. (2012). Randomized controlled split-mouth clinical trial of direct laminate veneers with two micro-hybrid resin composites. Journal of dentistry, 40(9), 766-775.
View at Publisher | View at Google Scholar - Heintze, S. D., Rousson, V., & Hickel, R. (2015). Clinical effectiveness of direct anterior restorations—A meta-analysis. Dental materials, 31(5), 481-495.
View at Publisher | View at Google Scholar - Hickel R, Roulet JF, Bayne S, Heintze SD, Mjör IA, Peters M, Rousson V, Randall R, Schmalz G, Tyas M, Vanherle G. Recommendations for conducting controlled clinical studies of dental restorative materials. Clin Oral Investig. 2007 Mar;11(1):5-33.
View at Publisher | View at Google Scholar - Hickel R, Peschke A, Tyas M, Mjör I, Bayne S, Peters M, Hiller KA, Randall R, Vanherle G, Heintze SD. FDI World Dental Federation - clinical criteria for the evaluation of direct and indirect restorations. Update and clinical examples. J Adhes Dent. 2010 Aug;12(4):259-72.
View at Publisher | View at Google Scholar - Karaman, E., Yazici, A. R., Ozgunaltay, G., & Dayangac, B. (2012). Clinical evaluation of a nanohybrid and a flowable resin composite in non-carious cervical lesions: 24-month results. Journal of Adhesive Dentistry, 14(5).
View at Publisher | View at Google Scholar - Kim, K. H., Ong, J. L., & Okuno, O. (2002). The effect of filler loading and morphology on the mechanical properties of contemporary composites. The Journal of prosthetic dentistry, 87(6), 642-649.
View at Publisher | View at Google Scholar - Kim, K. L., Namgung, C., & Cho, B. H. (2013). The effect of clinical performance on the survival estimates of direct restorations. Restorative Dentistry & Endodontics, 38(1), 11-20.
View at Publisher | View at Google Scholar - Loomans, B. A. C., Roeters, F. J. M., Opdam, N. J. M., & Kuijs, R. H. (2008). The effect of proximal contour on marginal ridge fracture of Class II composite resin restorations. Journal of Dentistry, 36(10), 828-832.
View at Publisher | View at Google Scholar - Lynch, C. D., Frazier, K. B., McConnell, R. J., Blum, I. R., & Wilson, N. H. F. (2010). State-of-the-art techniques in operative dentistry: contemporary teaching of posterior composites in UK and Irish dental schools. British Dental Journal, 209(3), 129-136.
View at Publisher | View at Google Scholar - Manhart, J., Chen, H. Y., Hamm, G., & Hickel, R. (2004). Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. OPERATIVE DENTISTRY-UNIVERSITY OF WASHINGTON-, 29, 481-508.
View at Publisher | View at Google Scholar - Millar, B. J., Robinson, P. B., & Inglis, A. T. (1997). Clinical evaluation of an anterior hybrid composite resin over 8 years. British dental journal, 182(1), 26-30.
View at Publisher | View at Google Scholar - Mjör IA, Shen C, Eliasson ST, Richter S. Placement and replacement of restorations in general dental practice in Iceland. Oper Dent. 2002 Mar-Apr;27(2):117-23. PMID: 11931133.
View at Publisher | View at Google Scholar - Mondelli, J., Steagall, L., Ishikiriama, A., de Lima Navarro, M. F., & Soares, F. B. (1980). Fracture strength of human teeth with cavity preparations. Journal of Prosthetic Dentistry, 43(4), 419-422.
View at Publisher | View at Google Scholar - Moura, F. R. R. D., Romano, A. R., Lund, R. G., Piva, E., Rodrigues Júnior, S. A., & Demarco, F. F. (2011). Three-year clinical performance of composite restorations placed by undergraduate dental students. Brazilian dental journal, 22, 111-116.
View at Publisher | View at Google Scholar - Nagem Filho, H., Nagem, H. D., Francisconi, P. A. S., Franco, E. B., Mondelli, R. F. L., & Coutinho, K. Q. (2007). Volumetric polymerization shrinkage of contemporary composite resins. Journal of Applied Oral Science, 15, 448-452.
View at Publisher | View at Google Scholar - Namgung, C., Rho, Y. J., Jin, B. H., Lim, B. S., & Cho, B. H. (2013). A retrospective clinical study of cervical restorations: longevity and failure-prognostic variables. Operative dentistry, 38(4), 376-385.
View at Publisher | View at Google Scholar - Opdam, N. J., Bronkhorst, E. M., Roeters, J. M., & Loomans, B. A. (2007). A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dental materials, 23(1), 2-8.
View at Publisher | View at Google Scholar - Peumans, M., De Munck, J., Van Landuyt, K. L., Poitevin, A., Lambrechts, P., & Van Meerbeek, B. (2012). A 13-year clinical evaluation of two three-step etch-and-rinse adhesives in non-carious class-V lesions. Clinical oral investigations, 16, 129-137.
View at Publisher | View at Google Scholar - Poyser, N. J., Briggs, P. F. A., Chana, H. S., Kelleher, M. G. D., Porter, R. W. J., & Patel, M. M. (2007). The evaluation of direct composite restorations for the worn mandibular anterior dentition–clinical performance and patient satisfaction. Journal of oral rehabilitation, 34(5), 361-376.
View at Publisher | View at Google Scholar - Qin, W., Song, Z., Ye, Y. Y., & Lin, Z. M. (2013). Two-year clinical evaluation of composite resins in non-carious cervical lesions. Clinical oral investigations, 17, 799-804.
View at Publisher | View at Google Scholar - Reusens, B., D’hoore, W., & Vreven, J. (1999). In vivo comparison of a microfilled and a hybrid minifilled composite resin in Class III restorations: 2-year follow-up. Clinical Oral Investigations, 3, 62-69.
View at Publisher | View at Google Scholar - Ryge G. Clinical criteria. Int Dent J. 1980 Dec;30(4):347-58. PMID: 6935165.
View at Publisher | View at Google Scholar - Smales, R. J. (1991). Effects of enamel-bonding, type of restoration, patient age and operator on the longevity of an anterior composite resin. American journal of dentistry, 4(3), 130-133.
View at Publisher | View at Google Scholar - Van de Sande, F. H., Opdam, N. J., Da Rosa Rodolpho, P. A., Correa, M. B., Demarco, F. F., & Cenci, M. S. (2013). Patient risk factors’ influence on survival of posterior composites. Journal of dental research, 92(7_suppl), S78-S83.
View at Publisher | View at Google Scholar - Van Dijken, J. W., & Pallesen, U. (2008). Long-term dentin retention of etch-and-rinse and self-etch adhesives and a resin-modified glass ionomer cement in non-carious cervical lesions. Dental Materials, 24(7), 915-922.
View at Publisher | View at Google Scholar - Van Dijken, J. W., & Pallesen, U. (2010). Fracture frequency and longevity of fractured resin composite, polyacid-modified resin composite, and resin-modified glass ionomer cement class IV restorations: an up to 14 years of follow-up. Clinical oral investigations, 14, 217-222.
View at Publisher | View at Google Scholar - Van Meerbeek, B., De Munck, J., Yoshida, Y., Inoue, S., Vargas, M., Vijay, P., ... & Vanherle, G. (2003). Adhesion to enamel and dentin: current status and future challenges. OPERATIVE DENTISTRY-UNIVERSITY OF WASHINGTON-, 28(3), 215-235.
View at Publisher | View at Google Scholar - Van Noort, R., & Davis, L. G. (1993). A prospective study of the survival of chemically activated anterior resin composite restorations in general dental practice: 5-year results. Journal of Dentistry, 21(4), 209-215.
View at Publisher | View at Google Scholar - Wilder Jr, A. D., Swift Jr, E. J., Heymann, H. O., Ritter, A. V., Sturdevant, J. R., & Bayne, S. C. (2009). A 12-year clinical evaluation of a three-step dentin adhesive in noncarious cervical lesions. The Journal of the American Dental Association, 140(5), 526-535.
View at Publisher | View at Google Scholar - Willems, G., Lambrechts, P., Braem, M., Celis, J. P., & Vanherle, G. (1992). A classification of dental composites according to their morphological and mechanical characteristics. Dental Materials, 8(5), 310-319.
View at Publisher | View at Google Scholar